- Vol 67 No 02
- Volume 67
- Issue 02
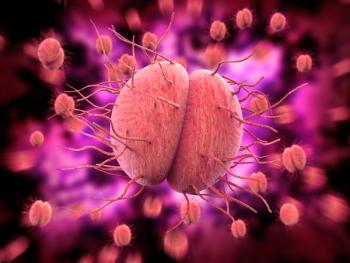
Ibrexafungerp vs fluconazole for vulvovaginal candidiasis
A recent study found ibrexafungerp (Brexafemme, Scynexis) was found to be a well-tolerated novel antifungal with similar efficacy to fluconazole for treating acute vulvovaginal candidiasis.
Oral ibrexafungerp (Brexafemme, Scynexis) was found to be a well-tolerated novel antifungal with similar efficacy to fluconazole for treating acute vulvovaginal candidiasis (VVC), according to a phase 2 randomized study in the journal Clinical Infectious Diseases.1
“There has been little change in the management of yeast infections since the approval of fluconazole in the early 1990s,” said senior author Paul Nyirjesy, MD, a professor of obstetrics and gynecology at Sidney Kimmel Medical College, Thomas Jefferson University, in Philadelphia, Pennsylvania, who noted that VVC affects roughly 75% of women in their lifetime.
“Meanwhile, there is clearly a need for better medications, not only for women with non-albicans Candida infections and recurrent and resistant C. albicans infections, but for those who develop side effects or allergy with fluconazole,” Nyirjesy told Contemporary OB/GYN®.
Ibrexafungerp, a triterpenoid glucan synthase inhibitor, has shown excellent in vitro activity for many yeasts that cause vaginal infections and penetrate vaginal tissues, according to Nyirjesy. “As such, it makes sense to conduct clinical trials to see if it can be an effective treatment for VVC,” he said.
The study comprised 186 patients with vulvovaginal signs and a symptoms score of greater than or equal to 7 who were randomized equally to 6 treatment groups. Five of the groups were administered different treatment doses of oral ibrexafungerp (750 mg for 1 day; 300 mg twice daily for 1 day; 450 mg twice daily for 1 day; 150 mg twice daily for 1 to 3 days; and 300 mg twice daily for 1 to 3 days) and 1 group was given oral fluconazole 150 mg for 1 day.
The major endpoint was the percentage of patients with a clinical cure (complete resolution of vulvovaginal signs and symptoms) at the test-of-cure visit at day 10.
Results were of the modified intent-to-treat population (baseline positive culture) for ibrexafungerp 300 mg twice daily for 1 day (n = 27) and fluconazole 150 mg for 1 day (n = 24).
At day 10, the clinical cure rates for ibrexafungerp and fluconazole were 51.9% and 58.3%, respectively, whereas at day 25, patients with no signs or symptoms were 70.4% and 50.0%, respectively.
During the study period, ibrexafungerp patients also required less antifungal rescue medications compared to fluconazole: 3.7% vs 29.2%, respectively.
In addition, ibrexafungerp was well tolerated, with the most common treatment-related adverse events being mild gastrointestinal events.
Nyirjesy, who was study site principal investigator at Drexel University in Philadelphia, where he was on faculty, is not surprised by the study’s findings. “It was nice to see that the drug was effective,” he said. “As a phase 2 dose-ranging study, it was underpowered to compare it to fluconazole, thus making all comparisons really descriptive.”
The results led to ibrexafungerp 300 mg twice daily for 1 day being selected as the dose for phase 3 studies, both of which were recently published in
However, because the phase 2 studies were not intended or powered to truly compare ibrexafungerp to fluconazole and because phase 3 studies assessed a single-day course, compared to placebo, “most of the advantages of ibrexafungerp are theoretical, such as being fungicidal and broad spectrum,” said Nyirjesy, co-director of the Jefferson Vulvovaginal Health Center at Thomas Jefferson University. “Nonetheless, the major clear advantage is that the drug offers a new effective therapy for women with acute VVC who cannot take oral fluconazole or do not wish to use an antifungal cream.”
Two barriers to adoption of ibrexafungerp, however, are the cost and that the drug should not be taken by women who may be pregnant.
“The main question remaining is what dose and duration of therapy will be needed for women with complicated yeast infections,” Nyirjesy said.
Disclosure:
Nyirjesy is a consultant and has been an investigator for studies sponsored by Scynexis and Mycovia Pharmaceuticals.
Reference:
1. Nyirjesy P, Schwebke JR, Angulo DA, et al. Phase 2 randomized study of oral ibrexafungerp versus fluconazole in vulvovaginal candidiasis. Clin Infect Dis. Published online September 23, 2021.
Articles in this issue
almost 4 years ago
How to provide excellent phone servicealmost 4 years ago
A noninfectious “infection” after cesarean deliveryabout 4 years ago
Statin use in midlife womenabout 4 years ago
Radiofrequency ablation for fibroidsabout 4 years ago
Tackling heart healthabout 4 years ago
Vaccination: Protecting our most vulnerableabout 4 years ago
Female contraception policies at US prisons and jailsabout 4 years ago
Midlife vision impairment and depressive symptomsNewsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.