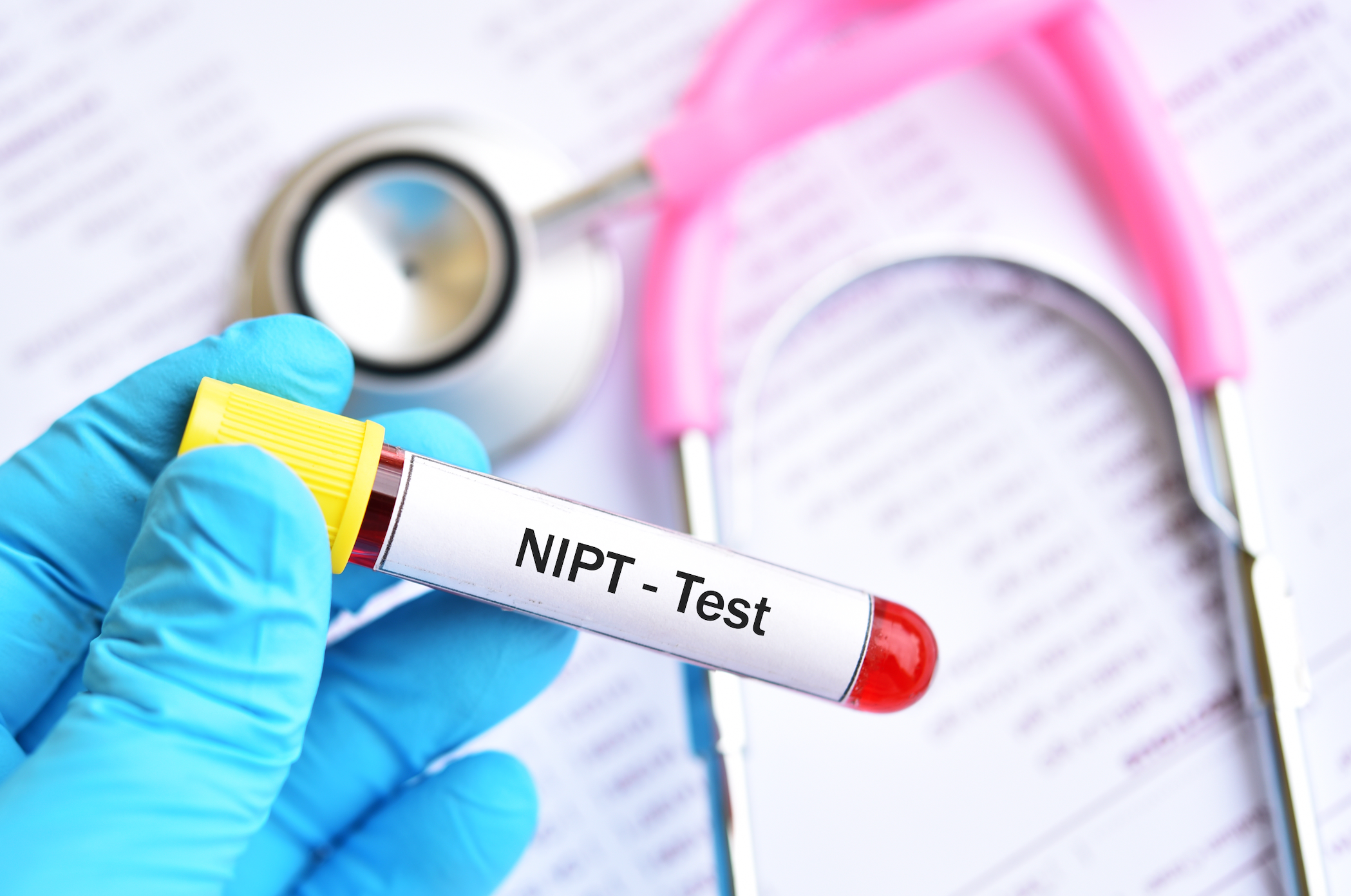
Noninvasive Prenatal Testing
Latest News

Latest Videos
CME Content
More News

A study in the journal Ultrasound in Obstetrics & Gynecology1 has found that noninvasive prenatal testing (NIPT) can help in the early detection of a set of single gene disorders (SGDs), especially in the presence of either abnormal ultrasound findings or a family history.

Pregnant women do not believe that noninvasive prenatal testing (NIPT) is an obligation of responsible motherhood, according to a qualitative study that investigated the impact of NIPT on women's moral beliefs about the meaning of prenatal screening.

Clinicians should carefully consider using noninvasive prenatal testing (NIPT) for the screening of chromosomal abnormalities in twin pregnancies because the combined positive predictive value (PPV) is limited and the screening efficiency is not stable, according to a prospective study.

Despite the inadvisability of performing early amniocentesis (EA) before 15 gestational weeks due to a high rate of miscarriage, a retrospective cohort study has found no significant difference in the procedure-related risk of miscarriage between EA, at around 14 weeks gestation, and mid-trimester amniocentesis (MA).

A retrospective analysis has found that comprehensive examination of shallow-sequenced, whole-genome cell-free DNA (cfDNA) allows for the incidental detection of maternal tumors, with relatively high precision.

The association between confined placental mosaicism (CPM) and prenatal growth and adverse pregnancy outcomes is significant, according to a literature review in the journal Human Reproduction Update.

A systematic review and meta-analysis on the benefits of non-invasive prenatal testing (NIPT) for detecting hemolytic disease of fetus and newborn (HDNF) validates routing anti-D prophylaxis.
An analysis of a large cohort of patients who chose noninvasive prenatal testing (NIPT) as a screening method for fetal trisomy 21, 18, and 13 (T21, T18 and T13) and sex chromosome aneuploidies (SCA) concluded there were extremely high detection rates and exceptionally low false positive rates.

Expanding coverage for noninvasive prenatal testing (NIPT) through a performance-based, risk-sharing agreement (PBRSA) resulted in a significant increase in NIPT use, a significant decrease in conventional prenatal screening methods, and a negligible increase in per member per month (PMPM) cost at Harvard Pilgrim Health Care (HPHC) in New England.

A small percentage of women whose noninvasive prenatal testing (NIPT) results were negative regretted taking the test and blamed themselves, according to a 1-year postpartum questionnaire survey.

A public health screening program for Down syndrome in Quebec, Canada, found that cell-free DNA noninvasive prenatal testing (NIPT) could be implemented at the same cost as the current screening program, according to computer simulations.

Some women are unable to choose noninvasive prenatal testing (NIPT), due to lack of insurance coverage, according to a pilot study in the Journal of Community Genetics.

Preimplantation genetic testing for aneuploidy (PGT-A) is not associated with a difference in risk of fetal anomaly detected on mid-trimester anatomical survey, according to a study.

“Our results can further inform the debate on the future uses of NIPT and future policy of its implementation,” said co-principal investigator Hazar Haidar, PhD, a lecturer in bioethics at Université du Québec à Montréal (UQAM), Montréal, Canada.

The investigators found an extremely low failure rate of 0.31%.

A population-based register study from the Netherlands has found that the percentage of pregnant women opting for fetal aneuploidy screening reached a high of 45.9% within 1 year after the introduction in 2017 of a noninvasive prenatal test (NIPT) as a first-tier test for all women.