Risk factors for development of PEP include rapid weight gain, multiple gestation pregnancy, nulliparous, and primigravid.2 It usually self-resolves in the postpartum period and does not recur with subsequent pregnancies.
Dermatoses of Pregnancy
Curbside Consults delivers expert perspectives from physicians outside of the OB/GYN specialty to provide insight into various health issues affecting pregnant women. This new section is the brainchild of Editorial Advisory Board member Christine Isaacs, MD.
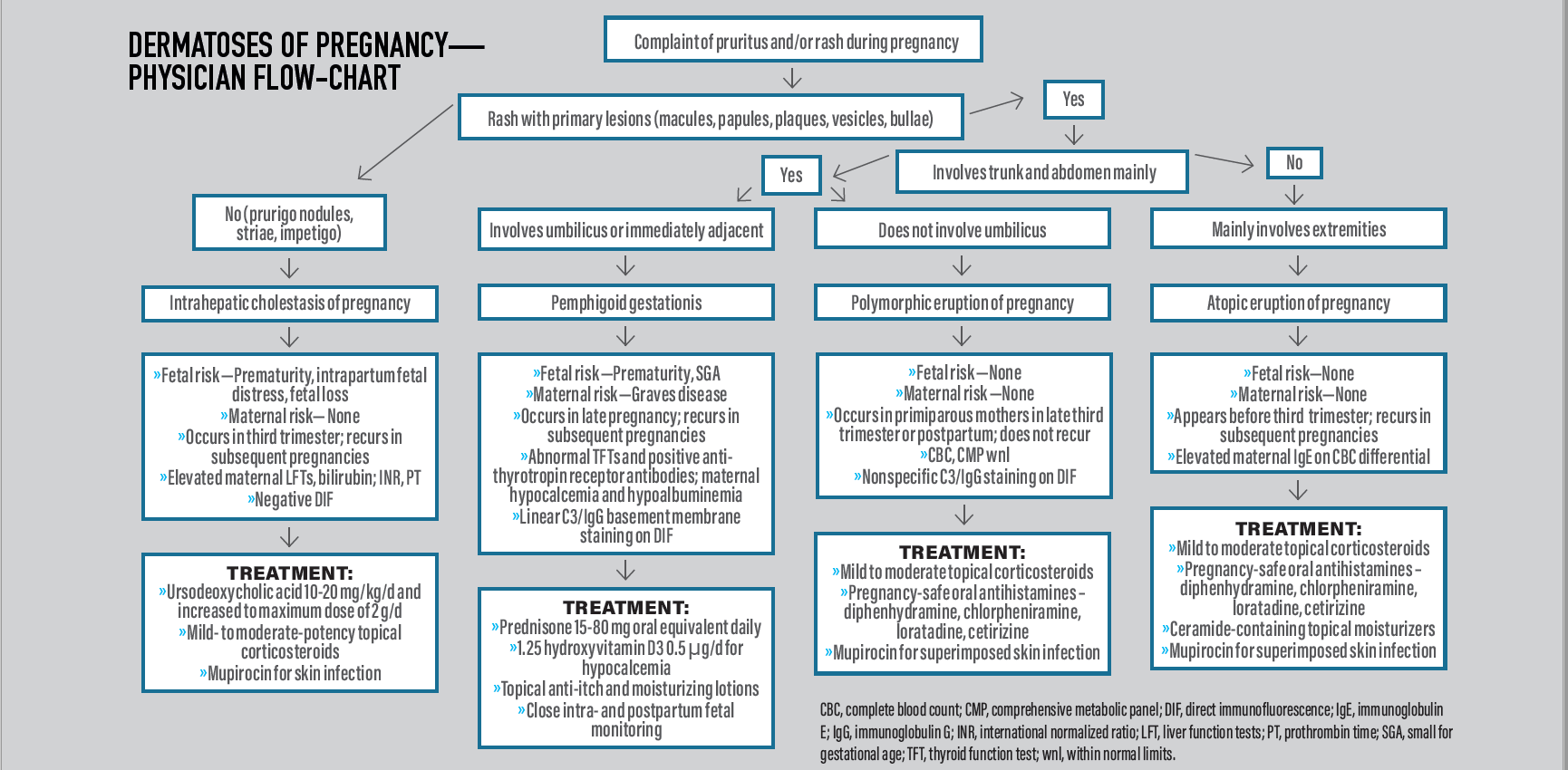
For an easy-to-use reference, print out this Dermatoses of Pregnancy Physician Flow Chart.
Scenario 1: The Itchy Stretch Marks
A 28-year-old primigravid patient presents for her routine prenatal visit. She is 36 weeks pregnant and complains that the stretch marks on her abdomen have become extremely itchy, red, and bumpy. She has no other obstetric complaints. Vital signs and fetal monitoring are within normal limits.
On physical exam you see this (Figure 1):
Figure 1. Multiple pink to red papules coalescing into plaques within striae on abdomen, consistent with polymorphic eruption of pregnancy.1

What should you do?
This scenario describes polymorphic eruption of pregnancy (PEP), also known as pruritic urticarial papules and plaques of pregnancy (PUPPP). Clinically, this presents as an abrupt onset of pruritic urticarial papules and plaques, targets, and vesicles within and around abdominal striae distensae, trunk, buttocks, and thighs. It typically spares the umbilicus, palms, and soles. There are no associated maternal or fetal morbidities.
Recommended initial management by obstetrician:
- Order complete blood count (CBC), liver function tests (LFTs), thyroid function tests (TFTs), and bile acids to rule out other dermatoses of pregnancy.2
- If necessary, perform two 3-0 punch biopsies, one from a papule or plaque for hematoxylin and eosin (H&E) staining and the other on perilesional uninvolved skin for direct immunofluorescence (DIF) studies. DIF will show nonspecific C3 staining of basement membrane and scant immunoglobulin (Ig) G staining in the epidermis, whereas H&E will show nonspecific lymphohistiocytic infiltrate in dermis, edema, and eosinophils.3
- Start mild to moderate topical corticosteroid and pregnancy-safe sedating or nonsedating oral antihistamines (diphenhydramine, chlorpheniramine, loratadine, cetirizine) to manage rash and pruritus.2
- Refer to dermatologist if rash becomes intractable.
Scenario 2: Blisters All Over My Belly
A 30-year-old primigravid patient at 37 weeks of pregnancy comes in complaining of itchy hives and blisters that suddenly developed on her abdomen and thighs. She denies fever, malaise, or any other systemic symptoms.
On physical exam you see this (Figure 2):
Figure 2. Multiple tense bullae on an erythematous urticarial base on the abdomen and thighs, consistent with pemphigus gestationis.4

What should you do?
This scenario describes pemphigoid gestationis, also known as herpes gestationis, which typically presents in late pregnancy or the postpartum period as an abrupt onset of PUPP that progress to tense vesicles and bullae on an erythematous base. Of note, these lesions involve the umbilicus or are immediately adjacent to it and spread to extremities, including palms and soles. Fetal risks include prematurity and small for gestational age.5 Maternal risks include Graves disease.5 Early-onset disease correlates with disease severity. This usually self-resolves during the postpartum period but can recur in subsequent pregnancies.
Herpes gestationis typically presents in late pregnancy or the postpartum period.
Recommended initial management by obstetrician:
- Take two 4-0 punch biopsies, one from a vesicle for H&E staining and the other from perilesional uninvolved skin for DIF. H&E will show a subepidermal blister and eosinophilic spongiosis, whereas DIF will show linear C3/IgG staining along the basement membrane.6
- Check TFTs to monitor for maternal risk of Graves disease, and perform a fetal non-stress test ultrasound for fetal monitoring.
- Treat with moderate- to high-potency topical corticosteroids and oral antihistamines. The mainstay of treatment is 20 to 60 mg oral prednisone equivalent daily, with taper after blisters disappear.6
- Refer to dermatology and endocrinology departments for further management.
Scenario 3: Itchy Rash From Head to Toe
A 21-year-old woman at 12 weeks of pregnancy presents with a complaint of new itchy bumps that started a week ago on her face and neck, under her arms, under her breasts, and on her arms and legs. She reveals she has never had a rash like this but did have eczema as a child. She does not complain about any other symptoms. Vital signs and fetal monitoring are within normal limits.
On physical exam you see the following (Figure 3):
Figure 3. Multiple excoriated papules on bilateral thighs, consistent with atopic eruption of pregnancy.7

What should you do?
This scenario describes atopic eruption of pregnancy, which is the most common rash seen in pregnancy. Onset is typically before the second or third trimester. It is a spectrum of conditions that includes prurigo of pregnancy, eczema of pregnancy, and pruritic folliculitis of pregnancy.
Clinically, it presents as excoriated papules or nodules, eczematous papules and plaques, or monomorphic follicular-based papules on the abdomen, flexural areas, and extremities. It typically occurs in patients with a history of atopic dermatitis but could be of new onset. It is due to an immune system shift from a T-helper (Th)1-predominant to a Th2-predominant system during pregnancy.
Patients who already have this imbalance due to atopic dermatitis experience flares. It is self-limited and there are no maternal or fetal risks.
Recommended initial management by obstetrician:
- Rule out other potentially severe conditions such as intrahepatic cholestasis of pregnancy and pemphigoid gestationis, scabies, pityriasis rosea, drug eruptions, and viral exanthems, which can present similarly.
- Perform punch biopsies for H&E staining and DIF. Order CBC, comprehensive metabolic panel (CMP), and TFTs. CBC will show elevated IgE.7
- Treat rash with moisturizers and emollients rich in ceramides, mild to moderate topical corticosteroids, oral antihistamines, and narrow band UV-B.7
- Culture lesions if any sign of infection is present and prescribe daily topical mupirocin once infection is confirmed.
Scenario 4: The Itchy Arms and Legs
A 22-year-old gravida 2 para 1 woman at 33 weeks of pregnancy presents with the complaint that she has been itchy all over her body for the past 3 days. She states that itching prevents her from sleeping at night and she experienced something similar during her first pregnancy but not as intensely. She reports that her first child was born at 35 weeks. Physical exam shows normal-appearing skin without any rash or secondary lesions
What should you do?
This scenario describes intrahepatic cholestasis of pregnancy, which is characterized by extreme pruritus in absence of rash, followed by secondary excoriation and prurigo papules and nodules. There is no long-term morbidity to the mother, but fetal risks include premature birth, meconium staining of amniotic fluid, abnormal fetal heart rate, and stillbirth.8 This condition is self-limited, with itching resolving days after delivery. It recurs with subsequent pregnancies.
Recommended initial management by obstetrician:
- Check CBC; CMP, with a focus on aspartate aminotransferase, alanine aminotransferase, and bilirubin; prothrombin time; activated partial thromboplastin time; international normalized ratio; hepatitis C; and genetic testing for genetic mutations in various hepatobiliary bile transporters.
- Monitor fetus for fetal anoxia caused by toxic bile crossing the placenta.
- Prescribe ursodeoxycholic acid 10 to 20 mg/kg/d and increase to maximum dose of 2 g/d.8
- Prescribe anti-itch over-the-counter emollients and moisturizers and topical corticosteroids.
- Culture erosions if infection is suspected and prescribe topical mupirocin ointment once infection is confirmed.
Scenario 5: The Pus-Filled Rash
A 25-year-old woman at 30 weeks of pregnancy presents with complaint of new-onset rash located in her axilla and groin, as well as malaise and fever. She states that she has never had a rash like this.
On physical exam you note the following (Figure 4):
Figure 4. Multiple pink, annular, scaly plaques with surrounding sterile pustules on arms, chest, and abdomen, consistent with impetigo herpetiformis.9

What should you do?
This scenario presents a case of impetigo herpetiformis, also known as generalized pustular psoriasis of pregnancy. This presents in the third trimester of pregnancy as eczematous scaly plaques surrounded by 1- to 3-mm pustules in flexural areas, which then extend to the trunk and extremities.
Patients usually have no prior history of psoriasis. Maternal risk includes seizures, tetany, delirium, and cardiac arrhythmias secondary to hypocalcemia.10 Fetal risk includes placental insufficiency.10 The condition typically self-resolves in the postpartum period, and it recurs with earlier onset and a more severe course in subsequent pregnancies.
Recommended initial management by obstetrician:
- Check CBC for elevated white blood cell count; check CMP for hypocalcemia and hypoalbuminemia.
- Perform 2 punch biopsies for DIF and H&E. DIF will be negative for any immunoglobulins.
- Counsel patient on natural progression of disease, with potential for early delivery if condition becomes life-threatening.
- Treat rash with systemic corticosteroids with a starting dose of prednisone 15 to 80 mg oral equivalent daily; replace deficient electrolytes; prescribe 1.25 hydroxyvitamin D3 0.5 µg/d for hypocalcemia; and supplements for hypoalbuminemia.10,11
- Consider referral to dermatologist for refractory cases.
- Follow up in 2 weeks to a month for fetal monitoring.
Scenario 6: The Bleeding Bump on the Lip
A 36-year-old woman at 29 weeks of pregnancy presents with a complaint of a bleeding bump on her lip. She does not recall any trauma to her lip and states the lesion started growing slowly over the past month. She has not attempted any home remedies and complains of no other symptoms. Her physical exam and fetal monitoring are within normal limits.
In physical exam you see the following (Figure 5):
Figure 5. A solitary red, dome-shaped papule on the lower lip, indicative of a pyogenic granuloma.

What should you do?
This case scenario describes a pyogenic granuloma, also known as pregnancy granuloma, which is a vascular lesion composed of multiple capillary hemangiomas. Its development is associated with increasing hormonal levels in pregnancy, as well as trauma.12
It presents as a dome-shaped, painful, hemorrhagic papule usually on the gingiva, but it can also occur on the lips and other bodily sites. Their presence can cause pain, anxiety, difficulty eating, and, though rarely, life-threatening hemorrhage if poorly controlled.
Recommended initial management by obstetrician:
- Evaluate for size, pain, and frequency of bleeding to guide the next best step in treatment.
- Noninvasive treatment options include cryotherapy with liquid nitrogen, intralesional injection of triamcinolone 2.5 mg/mL, sclerotherapy, pulse dye laser, or neodymium-doped yttrium aluminum garnet laser treatment. Advise patient that multiple treatment sessions may be necessary.12
- Invasive treatment options include surgical excision, which is considered the standard of care but bears the risk of morbidity, deformity, and incomplete excision.
- Advise patient about the importance of maintaining good oral hygiene to prevent secondary infection of the lesion.
__
References
- Rudolph CM, Al-Fares S, Vaughan-Jones SA, Müllegger RR, Kerl H, Black MM. Polymorphic eruption of pregnancy: clinicopathology and potential trigger factors in 181 patients. Br J Dermatol. 2006;154(1):54-60. doi: 10.1111/j.1365-2133.2005.06856.x
- Bechtel, MA. Pruritus in pregnancy and its management. Dermatol Clin. 2018;36(3):259-265. doi:10.1016/j.det.2018.02.012
- Matz H, Orion E, Wolf R. Pruritic urticarial papules and plaques of pregnancy: polymorphic eruption of pregnancy (PUPPP). Clin Dermatol. 2006;24(2):105-108. doi:10.1016/j.clindermatol.2005.10.010
- Sävervall C, Sand FL, Thomsen SF. Pemphigoid gestationis: current perspectives. Clin Cosmet Investig Dermatol. 2017;10:441-449. doi:10.2147/CCID.S128144
- Engineer L, Bhol K, Ahmed AR. Pemphigoid gestationis: a review. Am J Obstet Gynecol. 2000;183(2):483-491. doi:10.1067/mob.2000.105430
- Hallaji Z, Mortazavi H, Ashtari S, Nikoo A, Abdollahi M, Nasimi M. Pemphigoid gestationis: clinical and histologic features of twenty-three patients. Int J Womens Dermatol. 2017;3(2):86-90. doi:10.1016/j.ijwd.2016.11.004
- Roth MM, Cristodor P, Kroumpouzos G. Prurigo, pruritic folliculitis, and atopic eruption of pregnancy: facts and controversies. Clin Dermatol. 2016;34(3):392-400. doi:10.1016/j.clindermatol.2016.02.012
- Marschall HU. Management of intrahepatic cholestasis of pregnancy. Expert Rev Gastroenterol Hepatol. 2015;9(10):1273-1279. doi:10.1586/17474124.2015.1083857
- Kondo RN, Araújo FM, Pereira AM, Lopes VCH, Martins LMM. Pustular psoriasis of pregnancy (impetigo herpetiformis)--case report. An Bras Dermatol. 2013;88(6 suppl 1):186-189. doi:10.1590/abd1806-4841.20132134
- Murase JE, Heller MM, Butler DC. Safety of dermatologic medications in pregnancy and lactation, I: pregnancy. J Am Acad Dermatol. 2014;70(3):401.e1-14, quiz 415. doi:10.1016/j.jaad.2013.09.010
- Namazi N, Dadkhahfar S. Impetigo herpetiformis: review of pathogenesis, complication, and treatment. Dermatol Res Pract. 2018:5801280. doi:10.1155/2018/5801280
- Tsai KY, Wang WH, Chang GH, Tsai YH. Treatment of pregnancy-associated oral pyogenic granuloma with life-threatening haemorrhage by transarterial embolisation. J Laryngol Otol. 2015;129(6):607-610. doi:10.1017/s0022215115001176
Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.
S4E1: New RNA platform can predict pregnancy complications
February 11th 2022In this episode of Pap Talk, Contemporary OB/GYN® sat down with Maneesh Jain, CEO of Mirvie, and Michal Elovitz, MD, chief medical advisor at Mirvie, a new RNA platform that is able to predict pregnancy complications by revealing the biology of each pregnancy. They discussed recently published data regarding the platform's ability to predict preeclampsia and preterm birth.
Listen