Endometriosis patients more likely to take opioids after surgery
A recent study highlights that patients with endometriosis undergoing laparoscopic surgery use more opioids postoperatively, suggesting the need for tailored pain management.
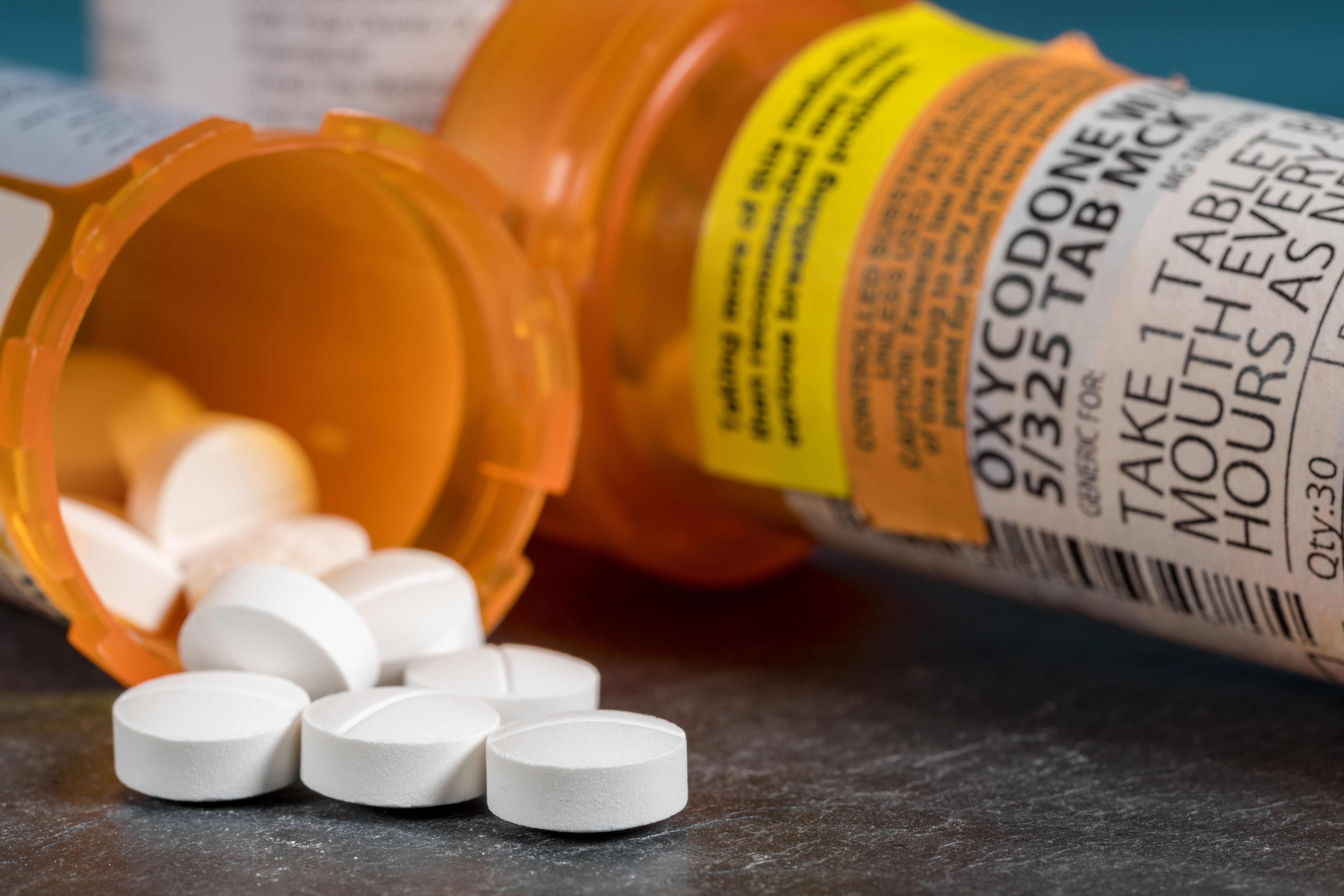
Higher post-surgery opioid use in endometriosis patients reported | Image Credit: © steheap - © steheap - stock.adobe.com.Higher post-surgery opioid use in endometriosis patients reported | Image Credit: © steheap - © steheap - stock.adobe.com.
Patients with endometriosis use post-operative morphine more frequently following laparoscopic surgery despite no significant differences in mean visual analogue scale (VAS) scores, according to a recent study published in Plos One.1
Gynecologic surgeries are often minimally invasive, especially when used to treat endometriosis. To manage postoperative pain, the enhanced recovery after surgery (ERAS) pathway is often employed, utilizing non-opioid analgesics and supplemental opioid analgesics.2
Approximately 10% of reproductive-aged women experience endometriosis, leading to symptoms such as dysmenorrhea, cyclic dysuria, lower abdominal pain, dyschezia, and dyspareunia.1 The inflammatory process of endometriosis often leads to hypersensitivity to pain in patients, with hormone therapy responses often inadequate.
As deep infiltrating lesions in the posterolateral parametria have been linked to central sensitization, researchers have hypothesized other variables may significantly impact central sensitization. Pain mechanisms in endometriosis patients are complex and vary between patients, highlighting the need for tailored pain management.
To evaluate pain perception and analgesic use following minimally invasive laparoscopic surgery vs laparoscopic hysterectomy in endometriosis patients, investigators conducted a retrospective cohort study. Participants included women receiving laparoscopic endometriosis surgery from 2019 to 2022 at Meir Medical Center.
A clinical evaluation including physical examination and ultrasound data was used to determine patients’ preoperative diagnoses. The American Society for Reproductive Medicine Endometriosis Classification System was used to diagnose stage 3 and stage 4 endometriosis.
Women receiving simple laparoscopic hysterectomy with salpingectomy, endometrial hyperplasia, or cervical intraepithelial neoplasia 3 were controls. Exclusion criteria included adenomyosis, malignancies indicating laparoscopic hysterectomy, and undergoing other benign gynecologic procedures.
The same surgical team conducted all laparoscopic surgeries for the study group. The same standard steps were used during surgery across both groups.
Demographic information, menstrual characteristics, preoperative symptoms, preoperative examination findings, and post-operative data were obtained from electronic medical records.Post-operative outcomes included VAS scores, hospitalization length, hemoglobin and white blood cell levels, and postoperative complications. VAS scores ranged from 0 to 10, with higher numbers indicating greater pain.
The ERAS program included pain relief analgesia on post-operative day (POD) 0 to 1. Patients’ need for pain medication and the type and dosage of any additional medication used was evaluated. Data was compared between patients with laparoscopic endometriosis surgery vs laparoscopic hysterectomy.
There were 200 women included in the final analysis, 100 in the endometriosis group and 100 in the control group. Excision of a sacro-uterine ligament endometriosis lesion occurred in 88% of the study group, excision of rectovaginal nodules in 55%, treatment for ovarian endometrioma in 65%, and excision of bladder endometriosis in 10%.
Patients with endometriosis were often younger and had reduced parity, but smoking and comorbidity characteristics did not significantly differ between groups. Dysmenorrhea, dyspareunia, and alterations in bowel movements were all more frequent in the endometriosis group.
Uterine tenderness, frozen pelvis, and ovarian mass were all more frequent in the study group, at rates of 25%, 3%, and 58%, respectively, vs 15%, 0%, and 25%, respectively among controls. However, menorrhagia and irregular menstrual cycles rates were increased in the control group, and the mean preoperative uterus size was larger.
Mean post-operative VAS scores did not significantly differ between groups, but a higher trend in mean VAS scores was identified in the endometriosis group between PODs 0 and 2. The use of full analgesic dosages within the standard protocol was observed more often in this group.
Ten percent of patients needing additional analgesics on POD1 in the study group used opioids rather than milder analgesics vs 1% in the control group. Rates of post-operative complications did not significantly differ between groups. An association was reported between morphine use on POD1 with more frequent use in the study group, with an odds ratio of 4.8
These results indicated increased use of opioid-based pain medication among endometriosis patients receiving laparoscopic resection of endometriosis lesions. Investigators concluded, “a customized analgesic regimen may be necessary for these patients.”
References
- Yagur Y, Engel O, Burstein R, et al. Pain after laparoscopic endometriosis-specific vs. hysterectomy surgeries: A retrospective cohort analysis. PLoS ONE. 2024;19(10):e0301074. doi:10.1371/journal.pone.0301074
- Nelson G, Altman AD, Nick A, et al. Guidelines for postoperative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations—Part 2. Gynecol Oncol. 2016;140: 323–332. doi:10.1016/j.ygyno.2015.12.019

Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.
