After decades of disappointments, a new generation of male contraceptives is under development and expected to enable men to share the contraceptive burden with their female partners. Many women and men are ready for this shift, experts tell Contemporary OB/GYN. But first, developers must address obstacles including misconceptions, funding challenges, and regulatory uncertainty.
Takeaways
- Male contraceptives offer the potential for a significant shift in reproductive responsibility between partners, enabling more equitable sharing of contraceptive duties, regardless of gender.
- Surveys suggest that around two-thirds of women desire more equitable sharing of contraceptive responsibilities, indicating substantial support for the development and adoption of male contraceptives.
- Many individuals, particularly women, experience dissatisfaction or adverse effects with existing contraceptive methods, emphasizing the need for a wider range of options to meet diverse needs and preferences.
- While concerns about trust exist, surveys indicate that a majority of women are likely to trust their male partners to use new male contraceptives as directed, with potential advantages in confirming efficacy through semen analysis.
- Despite progress, challenges such as funding limitations, regulatory uncertainties, and biases within the medical community remain significant barriers to the development and widespread adoption of male contraceptives, highlighting the need for continued efforts to overcome these obstacles.
A question of equity
“The most monumental change that’s going to come from male contraception is the ability for couples to have practical conversations about who’s going to use contraception and shared reproductive responsibility, independent of gender,” said Brian T. Nguyen, MD, MSc. He is an associate professor of clinical obstetrics and gynecology and assistant program director for the Fellowship in Complex Family Planning, Department of Obstetrics and Gynecology, at Keck School of Medicine, University of Southern California in Los Angeles.
Although studies of female attitudes toward male contraception are scarce, women’s eagerness for men to share the contraceptive burden appears substantial. In data from international surveys, around two-thirds of women have expressed a desire for more equitable sharing of contraceptive duties.1,2
Mitchell D. Creinin, MD, said, “Many patients have tried various different contraceptives, and they don’t work for them.” He is a professor and the director of the Complex Family Planning Fellowship in the Department of Obstetrics and Gynecology at University of California, Davis Health in Sacramento, California.
Many women dislike how oral contraceptives make them feel, Creinin said, yet they take them to avoid pregnancy. “Copper IUDs [intrauterine devices] significantly increase the amount of bleeding and cramping they get with their periods. And what I hear from patients is, ‘I can put up with it.’”
Even patients who are satisfied with their current contraceptive might want to discontinue it someday, added Nguyen. “And that’s where we hope that men can step in.”
According to men enrolled in a phase 2b trial of segesterone acetate (Nestorone; Population Council)–testosterone gel, in which he and Creinin are investigators, many are ready to step up (for more information, see sidebar). “They see what their partners go through, whether it be hormonal [adverse] effects, childbirth, or a pregnancy scare, and they want to take on some of the responsibility,” said Nguyen.
On a broader scale, data from the Male Contraceptive Initiative (MCI) show that the proportion of American men willing to take a male contraceptive in its first year of availability grew from 39% pre–Dobbs v Jackson Women’s Health Organization to 49% after the Roe v Wade reversal.3
A matter of trust
The big question, experts say, is whether women will trust men to use new male contraceptives as directed. Historically, said Nguyen, the perception has been that women remain skeptical. “But when we look at population surveys, we don’t see that.” In one such survey, only 2% of women said they would not trust their partner to use male contraception.1
At press time, Nguyen was conducting similar surveys of young US women. “Our preliminary results indicate that very few would not trust their male partners,” he said.
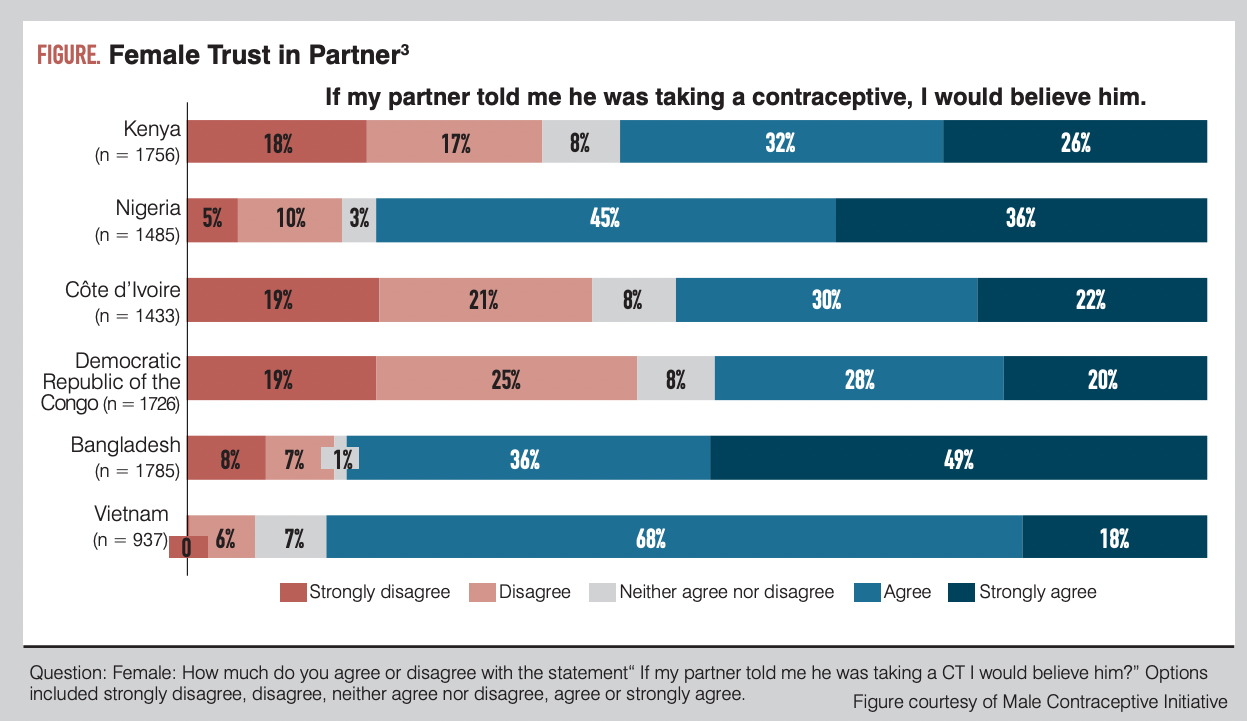
Likewise, when MCI asked more than 9000 women in 6 nations outside the United States how likely they were to believe their male partner if he said he was taking a contraceptive (Figure),3 the vast majority said they were likely or strongly likely. Agreement was highest in Vietnam (86%) and Bangladesh (85%).
Although no test can prove whether a woman is taking birth control pills daily, said Nguyen, one advantage of male contraceptives is that semen counts can confirm whether they are working. “If you want proof, you can get proof.”
Hormonal male contraceptives
Over the years, many hormonal projects achieved high efficacy but were abandoned due to unwanted adverse effects.4-6 However, Nguyen says that because hormonal contraceptives have been studied since the 1960s, physicians have the most confidence in their reversibility. Creinin added that due to the difficulties of developing nonhormonal contraceptives, hormonal methods will be first in line, possibly within 5 years in the United States.
Hormonal candidates still being investigated include dimethandrolone undecanoate and 11ß-methyl-19-nortestosterone 17ß-dodecyl carbonate.7 However, MCI Executive Director Heather Vahdat, MPH, said that because clinical studies might require several years’ ramp-up and follow-up, a male “pill” or longer-acting injectable hormones could be 10 years away.
Nonhormonal projects
“There’s a joke that male contraceptives have been 10 years away for 50 years,” said Vahdat. However, she noted, a solid chance exists—assuming all goes well—that a vas-occlusive product or products could reach the US market within 5 years.
Vas-occlusive products funded by MCI, which focuses on nonhormonal contraceptives, include the following:
- Adam (Contraline)—In a 23-patient phase 1 trial conducted in Australia, participants achieved 99.8% to 100% reductions in motile sperm (comparable to vasectomy) within 30 days of implantation.8
- Plan A (NEXT Life Sciences, Inc)—In January, NEXT announced $2.5 million in funding to support clinical research expected to begin in 2024’s first half. The company has announced plans for FDA submission in late 2024.9
Additional projects funded by MCI range from the retinoic acid receptor–alpha inhibitor YCT-529 (YourChoice Therapeutics), which entered a phase 1 trial in the United States late in 2023,10 to a band designed to raise testicular temperature.11
Remaining challenges
“The elephant in the room is funding,” said Vahdat. “With the amount of grant money that we put out every year ($1.5 million), MCI is the second-largest funder of male contraception in the world, which we’re very proud of. But it also highlights how underfunded the space is.” Therefore, MCI works closely with funding colleagues to ensure that grantees are poised to snag National Institutes of Health grants.
Beyond funding, said Vahdat, the regulatory pathway looms. “There’s no guidance at this point specific to male contraception,” she explained. Presently, she said, the people trying to address this barrier in the United States are “piecemealing” between FDA guidance for female contraceptives and relevant recommendations such as those regarding testicular toxicity. This approach could result in inconsistent requirements for different male contraceptive categories, Vahdat noted.
Additional obstacles may be less tangible. Nguyen added that obstetrician-gynecologists (ob-gyns) often manage unintended pregnancies and see situations where men may not use contraception correctly. These observations might fuel a bias that could impact the runway for male contraception, he said. “If pharmaceutical companies don’t believe that ob-gyns will welcome male contraception, they’re not going to put money behind it.”
Creinin said, “I think of my potential grandchildren growing up in an environment where male contraception is the norm.” Just as women not in sexual relationships may take birth control pills just in case, he noted, men one day will have the same option. “It’s a societal shift that will only occur once there’s a method available.”
References
1. Glasier AF, Anakwe R, Everington D, et al. Would women trust their partners to use a male pill? Hum Reprod. 2000;15(3):646-649. doi:10.1093/humrep/15.3.646/
2. Reed S, Sheng M, Patil D, Mehta A. Female attitudes toward male contraception. Fertil Steril. 2023;120(4):E243-E244. doi:10.1016/j.fertnstert.2023.08.687
3. Kretschmer S. Research assessing demand for novel male & female CTs in development. Presented at: 2023 National Contraception Meeting; November 13-16, 2023; Houston, TX.
4. Behre HM, Zitzmann M, Anderson RA, et al. Efficacy and safety of an injectable combination hormonal contraceptive for men. J Clin Endocrinol Metab. 2016;101(12):4779-4788. doi:10.1210/jc.2016-2141
5. Turner L, Conway AJ, Jimenez M, et al. Contraceptive efficacy of a depot progestin and androgen combination in men. J Clin Endocrinol Metab. 2003;88(10):4659-4667. doi:10.1210/jc.2003-030107
6. Balbach M, Rossetti T, Ferreira J, et al. On-demand male contraception via acute inhibition of soluble adenylyl cyclase. Nat Commun. 2023;14(1):637. doi:10.1038/s41467-023-36119-6
7. Abbe CR, Page ST, Thirumalai A. Male contraception. Yale J Biol Med. 2020;93(4):603-613.
8. Contraline achieves promising early clinical trial results for novel male contraceptive. Contraline. January 4, 2024. Accessed February 2, 2024. https://www.contraline.com/news/c4OvrhbCosTzz18u299nO44#contraline-achieves-promising-early
9. The Family leads NEXT Life Sciences $2.5 million funding round for Plan A male birth control. News release. NEXT Life Sciences. January 16, 2024. Accessed February 2, 2024. https://www.einpresswire.com/article/681741895/the-family-leads-next-life-sciences-2-5-million-funding-round-for-plan-a-male-birth-control
10. YourChoice Therapeutics begins first-in-human trial for male birth control pill. News release. YourChoice Therapeutics, Inc. December 13, 2023. Accessed February 2, 2024. https://www.pharmacy.umn.edu/news/yourchoice-therapeutics-begins-first-human-trial-male-birth-control-pill
11. Joubert S, Tcherdukian J, Mieusset R, Perrin J. Thermal male contraception: a study of users’ motivation, experience, and satisfaction. Andrology. 2022;10(8):1500-1510. doi:10.1111/andr.13264