Payment models put the value in value-based care
In this month's Practice Matters column, James D. Keller, MD, MHSA; and Brian K. Iriye, MD, explore the world of value-based care and how it can benefit your practice.
Value-based care | Image Credit: © leowolfert - © leowolfert - stock.adobe.com.

A quick Google search will yield roe than 2 billion results for “value-based care.” It has been covered in The New England Journal of Medicine, Harvard Business Review, and Obstetrics and Gynecology. Even the last Practice Matters column in Contemporary OB/GYN® referenced value-based care as a tactic to future-proof your practice.1-4
There are several definitions of value-based care, but the premise is the same. It is a payment model where providers are not only paid based on the amount of health care services they provide but also on quality and outcomes, such as improving the health of the individual or community.
Intuitively, any scheme for value-based care must begin with a framework of what quality is. The National Academy of Medicine has developed a widely accepted approach that describes high-value health care as safe, timely, effective, efficient, equitable, and patient-centered—STEEEP for short.5 Once a framework is built for high-value care, models must be developed to tie payment to the achievement of quality. The rule of thumb for providers is that there is a continuum of risk from fee for service where no payment is based on value to full capitation or a provider-owned insurance product fails to control cost and provide high-value care, resulting in financial disaster for the provider. The continuum is usually depicted as the model in the Figure.2
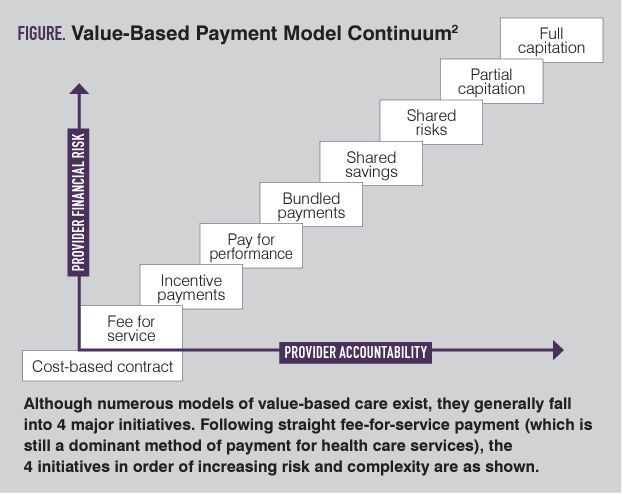
Although numerous models of value-based care exist, they generally fall into 4 major initiatives. Following straight fee-for-service payment (which is still a dominant method of payment for health care services), the 4 initiatives in order of increasing risk and complexity are as follows.
Performance incentives
In this model, providers are still paid for each volume of service provided but generally at a reduced rate compared with a classic fee-for-service model. Providers can then increase the revenue per episode for a defined duration of time by meeting quality metrics. This model requires goals to be set with clear expectations and definitions of how each goal is incentivized. Although this seems like a relatively straightforward model, just like all value-based incentives, there needs to be a robust platform for data collection along with risk stratification to avoid the unintended consequence of providers avoiding caring for populations where the reward thresholds cannot be met because of patient or population complexity.
Bundles
In this model, there is generally a payment tied to a particular procedure or management of a condition. For example, pregnancy can highlight the risks and benefits of such an approach. If a payer provides a certain amount of money for the management of pregnancy from beginning to end, the payer’s risk is reduced by having an idea of the next 9 months of expenditure. The provider could be rewarded by developing innovative models of care, which could reduce visits or low-value imaging that may not be necessary. The downside is that if an increased intensity of care is needed and provisions have not been made in advance to manage such an occurrence, the provider may be left with either a low margin or worse, a loss of money in the provision of care. In general, bundles are best managed with a large volume of patients so that the effect of outliers are dampened. Alternatively, carveouts can be entertained for the provision of care for patients at higher risk.
Shared savings
This is an optimistic title, because it implies that there are always savings and no downside for the provider. However, this is not the case. In this model, the cost of care for an entire population is compared with a preset goal that is generally set by looking at historic data of similar providers and populations. If the cost of care for the population is less than the benchmark, then the payer and provider split the savings. In general, the more risk the provider takes, the greater the portion of savings they can keep. For example, unless a provider is willing to be responsible for a portion of the cost over benchmark, the amount of the savings they keep will be limited. This is one of the reasons that participation in shared savings programs tends to be limited to higher-performing groups with the infrastructure to provide high-value care. This creates an issue, because the benchmark is set by these high-participating institutions, making savings more difficult to achieve. The lower the benchmark, the higher the risk of exceeding the set cost and thus owing money.
Capitation
In this model, the payer receives a lump sum for the care of an entire population. This is the closest model to the provider being an insurer. Although there is a tremendous upside to organizations that can provide high-value care, there is a theoretical risk of providers acting as payers. Although we would like to believe that all decisions are made with the patient’s best interests in mind, the possibility in all models exists to reward a lower cost of care to incentivize restricting access to necessary care. This risk is greatest when the provider is responsible for the total cost of care for the patient. As we look at capitation as a way to shift dollars to providers for well-coordinated, higher-value care, it is hard not to notice that payers are more likely to move into the provider space and retain the premium dollar than for providers to move into the payer space.
Conclusion
Although this article began with a description of what high-value care is, there is no value in wasted expense. It is well known that fee-for-service models incentivize excess health care expenditures. These expenditures affect us all with government spending, but a significant portion of the cost is carried by employers. This shifts dollars away from employee compensation, and with deductibles and co-pays, it can affect the financial health of individuals. The move toward value-based care will also promote critical evaluation of new technology, tests, and clinical pathways to improve outcomes, decrease cost, and improve patient experience.
References:
- What is value-based healthcare? NEJM Catal Innov Care Deliv. 2017;3(1).
- Harrison M. A 5-point model for value-based health care. Harvard Business Review. October 23, 2019. Accessed March 1, 2023. https://hbr.org/2019/10/a-5-point-model-for-value-based-health-care
- Sudhof L, Shah NT. In pursuit of value-based maternity care. Obstet Gynecol. 2019;133(3):541-551. doi:10.1097/AOG.0000000000003113
- Iriye B, Keller J. How to future-proof your practice. Contemporary OB/GYN. February 7, 2023. Accessed February 21, 2023. https://www.contemporaryobgyn.net/view/how-to-future-proof-your-practice
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001.

Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.
Anger hurts your team’s performance and health, and yours too
October 17th 2024Anger in health care affects both patients and professionals with rising violence and negative health outcomes, but understanding its triggers and applying de-escalation techniques can help manage this pervasive issue.
Read More
