
Nearly a third of women in poor or fair health have been without health care during the COVID-19 pandemic. Even more worrisome, only half of uninsured women have been to an ob/gyn provider over the past 3 years.
Sandra Fyfe is a freelance writer for Contemporary OB/GYN.

Nearly a third of women in poor or fair health have been without health care during the COVID-19 pandemic. Even more worrisome, only half of uninsured women have been to an ob/gyn provider over the past 3 years.

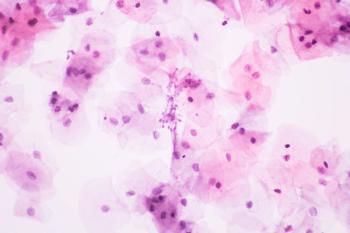
A Quest Diagnostics 2020 retrospective, longitudinal Health Trends Study® adds to previous research that shows co-testing is more effective than single testing alone.
The most significant finding is to watch for symptoms of VVC in women with T2D.

A new study led by Sejal Ajmera Desai, MD, MBBS, a consultant ob/gyn at the Indian Academy of Vaginal Aesthetics in Mumbai, India, found that women who received transcutaneous temperature-controlled radiofrequency treatment (TTCRF) saw substantial improvement in stress urinary incontinence (SUI), sexual dysfunction (SD), and female genital appearance. The most significant takeaway from this study for providers, according to study supervisor George Kroumpouzos, MD, PhD, FAAD, is that TTCRF is safe and effective.

Lower levels of testing and higher positivity rates, higher rates of dangerous drug combination use, and increases in fatal and non-fatal overdoses during the coronavirus disease 2019 (COVID-19) pandemic reveal a need for more resources to address the opioid epidemic in the United States.

Missing just 1 screening can lead to significant increase in risk, investigators say.

Women diagnosed with hypertensive disorders of pregnancy have an increased risk of premature mortality, particularly from cardiovascular disease.

A weekend workshop with a group therapy intervention program promoted safe sex and reduced drinking.

The scoping review revealed target areas that require additional research, as well as a need for more variety in study designs, populations, and locations.

Diverse Voices: COVID-19 and the Health of Women, a virtual speaker series run by the NIH Office of Research on Women’s Health (ORWH), presented compiled research on sex and gender disparities during the COVID-19 pandemic. In addition to identifying issues of concern, the webinar offered actions to improve women’s health despite sex and gender disadvantages.

A narrative review identified gaps in knowledge and considerations for informing sexually transmitted infection (STI) screening guidelines and treatment to improve the health of pregnant women and children.

Genitourinary Syndrome of Menopause is often overlooked by providers.

Researchers collected samples from 10 girls with vulvovaginitis and 16 healthy girls aged 3 to 9 years.
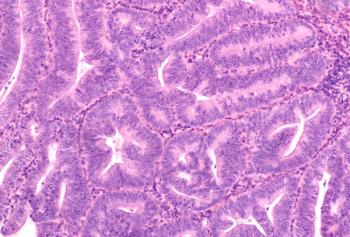
Total laparoscopic nerve-sparing radical hysterectomy (TL-NSRH) has advantages over open abdominal nerve-sparing radical hysterectomy (OA-NSRH), according to research published in the Journal of Gynecologic Oncology.

Women vaccinated following conization experienced a slightly lower, though not statistically significant, rate of recurrence of high-grade cervical dysplasia, according to a recent study.
Since radical hysterectomy does not improve survival, the procedure should be replaced with definitive chemoradiation, according to the ABRAX study published in the European Journal of Cancer.
While no difference was shown in disease-free survival rates between surgical and non-surgical staging methods, laparoscopy benefits patients with International Federation of Gynecology and Obstetrics (FIGO) stage IIB cervical cancer. Surgical staging also has a cancer-specific survival benefit, according to a study published in the International Journal of Gynecological Cancers.

With coronavirus disease 2019 limiting the availability of health resources, research using a comprehensive review and expert opinion has set pandemic treatment protocols for gynecological cancers.
“Reaching these women is critical to reduce cervical cancer rates.”
In the largest meta-analysis study to date, researchers find that a levonorgestrel-intrauterine system (LNG-IUS) used for 3 to 6 months is likely more effective than non‐intrauterine progestogens for reversing endometrial hyperplasia (EH).

Pregnant women with autoimmune-related interstitial lung disease (ILD) can have safe pregnancy outcomes if closely monitored by a multidisciplinary team of physicians.