
Adolescent oral contraceptive use is associated with a small yet meaningful increased risk of experiencing an episode of major depressive disorder (MDD) in early adulthood, especially among women with no history of MDD in adolescence.


Adolescent oral contraceptive use is associated with a small yet meaningful increased risk of experiencing an episode of major depressive disorder (MDD) in early adulthood, especially among women with no history of MDD in adolescence.

Among women with opioid use disorder (OUD) at high risk for unintended pregnancy, onsite contraceptive services coupled with financial incentives to attend follow-up visits to assess contraceptive satisfaction was a significantly more efficacious and cost-beneficial intervention than without incentives or with usual care, according to a prospective randomized clinical trial in JAMA Psychiatry.

A report indicates that both parents and teenagers want to have discussions on sexual and reproductive health during preventive visits, but those discussions may not be happening as often as they should be.

“Over the past several years, a growing number of companies have been providing contraception through online platforms, but there has been very little research on these businesses,” said principal investigator Brittni Frederiksen, MPH, PhD, a senior policy analyst at KFF in San Francisco.

An increasing number of pharmacists are now prescribing birth control, further expanding their role as public health service providers.

The authors of the prospective study in the journal Health Technology Assessment believe the simple intervention has enormous potential to prevent more unintended pregnancies after emergency contraception.
Significant updates occurred in women’s health issues while the world was in survival mode.

The new analysis, which was presented virtually at the 2021 American College of Obstetricians and Gynecologists (ACOG) Annual Clinical and Scientific Meeting, concludes that the TDS maintained similar safety and tolerability in the 2 groups of women.

Contrary to popular belief, emergency oral contraception is not that effective.

Early and routine contraceptive counseling for all women of reproductive age with cardiovascular disease or cardiovascular risk factors is an essential component of comprehensive cardiovascular care, according to evidence-based recommendations of contraceptive options published in the Journal of the American College of Cardiology (JACC).

Women with diabetes are slightly less likely to use contraception after their diabetes diagnosis, according to a retrospective cohort study in the journal Primary Care Diabetes.

Nextstellis (drospirenone; estetrol) now is approved as a combined oral contraceptive for birth control.

This video interview features Rachael Phelps, MD, Medical Director at Planned Parenthood of Central and Western New York, and of the Rochester LARC Initiative; and Amber Truehart, MD, Assistant Professor of Obstetrics and Gynecology, Section of Family Planning and Contraceptive Research at the University of Chicago.

A prospective study to assess the effects of an oral contraceptive containing estetrol and drospirenone on ovarian function found treatment achieved complete ovulation inhibition.
The pandemic has forced us to get more creative in managing patients’ needs, especially when it comes to contraception
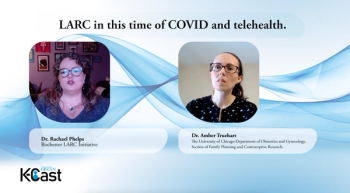
This video interview features Rachael Phelps, MD, Medical Director at Planned Parenthood of Central and Western New York, and of the Rochester LARC Initiative; and Amber Truehart, MD, Assistant Professor of Obstetrics and Gynecology, Section of Family Planning and Contraceptive Research at the University of Chicago.

In this episode, Dr. Rachel Phelps of the Rochester LARC Initiative sits down with Dr. Amber Trueheart of the University of Chicago Department of Obstetrics and Gynecology.

Limited changes occur in endocrine markers with the combined oral contraceptive Nextstellis (Mayne Pharma), according to a prospective study presented at the virtual annual meeting of the International Society for the Study of Women's Sexual Health (ISSWSH) in March.

Since 2012, when South Carolina's Medicaid program became the first state Medicaid program to separate payment for the immediate postpartum placement of long-acting reversible contraception (LARC) from global maternity payment, a significantly greater number of mothers are using LARC, especially among adolescents.

When it comes to willingness to switch contraception method, a team of researchers has looked into whether method type, satisfaction with use, and confidence in correct use were independently associated with switching intentions.

The mechanism of action (MOA) of emergency contraceptive pills (ECPs) is frequently mischaracterized among the general public, according to authors of a recent study published in the journal Contraception.

Three experts in maternal-fetal medicine hosted the Womxn’s Health Collaborative Symposium: Crucial conversations for careers in MFM during the Society for Maternal Fetal Medicine’s (SMFM) 41st Annual Pregnancy Meeting on Monday.

Initiation of more effective contraception occurred more often among patients who were seen by a volunteer reproductive health educator during routine visits at a resident obstetrics and gynecology clinic, according to a study published in Maternal and Child Health Journal.

In response to the coronavirus disease 2019 pandemic, many U.S. family planning providers have started offering telemedicine services.

The study in the Brazilian Journal of Nursing also found that the IUD complications were the same as those commonly cited in the literature.