
Many risk factors for fractures have been documented, including low bone-mineral density (BMD) and a history of fractures.

Many risk factors for fractures have been documented, including low bone-mineral density (BMD) and a history of fractures.

Urinary incontinence impacts 15 to 35% of the adult ambulatory population. Men after the removal of the prostate for cancer can experience incontinence for several weeks to years after the surgery.

Diagnostic discordance for osteoporosis is the observation that the T-score of an individual patient varies from one key measurement site to another, falling into two different diagnostic categories identified by the World Health Organization (WHO) classification system.

Obtaining reliable hemostasis is crucial as part of laparoscopically assisted vaginal hysterectomies, and over the past 20 years, various methods to do so have been advocated. For instance, in 1989, Harry Reich recommended using sutures to control the uterine vessels, as monopolar, bipolar, and laser instruments available at that time were inherently risky to use along the pelvic sidewall.
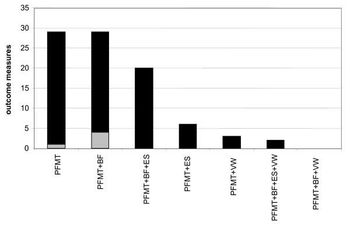
Stress urinary incontinence (SUI) is a prevalent and costly condition which may be treated surgically or by physical therapy.

High blood pressure complicates almost 10 percent of all pregnancies, and the incidence is higher if the women are nulliparous or carrying multiple fetuses.

In an extensive, multi-center clinical treatment trial, Canadian researchers evaluated the outcomes of 538 cases of uterine artery embolization for fibroids. Between 20% and 50% of women develop uterine fibroids, benign tumors in the muscular tissue of the uterus that can seriously impact their health and well-being.

This study was designed to determine whether epidural anesthesia would improve external cephalic version success in a safe and effective manner.

The ability to quickly, cost-effectively and accurately predict fetal pulmonary maturity would be a helpful adjunct in the management of problem pregnancies when either delivery or administration of glucocorticoid are management options.

Virtually half of the articles about genetic testing in the lay press contain the words "simple blood test". In a high-tech medical world of complicated imaging, medications and surgeries, reporters seem intrigued that much genetic testing can be performed on a blood specimen.

There are an increasing number of genetic disorders that can be diagnosed by direct DNA analysis, such as cystic fibrosis.

A recent survey of ob/gyns (N = 308) reported that respondents who indicated they had prior training in office uterine evacuation and/or induced abortion also reported using office uterine evacuation more frequently as compared to those providers without any training. The operation room was used more often by those respondents who did not have any induced abortion training.

In the newborn period, group B streptococcus agalactiae infection is the leading cause of sepsis in the United States. The overall attack rate of early onset GBS infection (EOGBSI) per 1000 deliveries ranges from 0.72 to 5.5.

It is implantation of the fertilised ovum outside the normal uterine cavity. Common site (95%) : the tubes. Rare sites (5%) : The ovaries, a rudimentary horn of a bicornuate uterus , broad ligaments, peritoneum and cervix.

Plasma renin activity (PRA) was determined by radioimmunoassay in maternal and cord blood of 20 women with pregnancy-induced hypertension (PIH) and in 20 normal pregnant controls.

On December 6, 1999, under Public Law 106-129, the Agency for Health Care Policy and Research (AHCPR) was reauthorized and renamed the Agency for Healthcare Research and Quality (AHRQ).

Of the nearly 4 million women giving birth in the United States each year, between 1 and 5 percent suffer from chronic hypertension.

Adapted from "The Ultrasound Detection of Chromosomal Anomalies

Labor at term is regarded as a release of the myometrium from the inhibitory effects of pregnancy (phase 0) which are mediated by a variety of suppressors that maintain uterine quiescence.

Formula feeding based on human milk composition

otohns.net Conference CoverageAnnual Meeting of the AAO-HNSF and Oto Expo Washington, D.C - 2000

These pages are designed to help parents to be. They cover the most common tests available to parents and include those which appear `routine' in every pregnancy. Parents are reminded that they should make their own mind up about which tests they need if any.

Molar pregnancies are an uncommon and very frightening complication of pregnancy. The formal medical term for a molar pregnancy is "hydatidiform mole."

With its accuracy, scope, and reproducibility, might transvaginal cervical imaging help us not only predict preterm labor but understand its mechanisms?

Although testosterone is generally considered to be a male hormone, it is produced in small amounts by the ovary. Other hormones with testosterone-like effects are also produced by both the ovary and the adrenal gland.

FDA approval for bevacizumab (Avastin) as treatment for metastatic HER2-negative breast cancer should be withdrawn, according to a unanimous vote (6-0) of the FDA’s Oncologic Drug Advisory Committee. The committee convened at the request of the drugmaker (Genentech) to appeal an earlier decision by the FDA to remove the indication for bevacizumab to treat locally recurrent or metastatic HER2-negative breast cancer.

Routine screening of pregnant women for vitamin D deficiency is not recommended, according to a new Committee Opinion of The American College of Obstetricians and Gynecologists. Although severe vitamin D deficiency during pregnancy has been linked with abnormal skeletal development, congenital rickets, and bone fractures in newborns, most pregnant women obtain enough vitamin D through prenatal vitamins, fortified milk and juice, fish oils, and sunlight exposure.

The most effective forms of reversible contraception available to date are long-acting reversible contraceptives (LARCs), which include intrauterine devices (IUDs) and implants.1 According to The American College of Obstetricians and Gynecologists (The College), LARCs are safe for almost all women of reproductive age, including nursing mothers, adolescents, and women who have not yet had a child, and The College recommends them as first-line contraceptive methods.

Transperineal and transabdominal sonography were done for 180 patients attending Benha University Hospitals at 28-40 weeks gestational age with an antepartum hemorrhage in the period between July, 1995 and October, 1996.

Pre-eclampsia is a disease of pregnancy characterized by Hypertension, proteinurea and edema. It is a multisystem disorder affecting virtually every organ and system in the body.