Exploring Ibrexafungerp for the Treatment of Vulvovaginal Candidiasis
Michael L. Krychman, MD, and Jack D. Sobel, MD, review the mechanisms of ibrexafungerp and how it might fit in the treatment spectrum for RVVC.
Episodes in this series

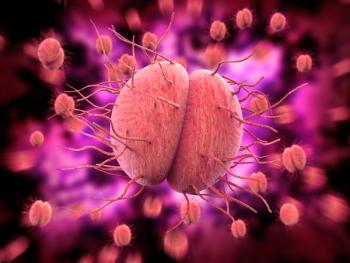
Michael L. Krychman, MD: I want to shift gears and talk about ibrexafungerp, which is a glucan synthase inhibitor. It’s fungicidal. I know you’re very familiar with it. It’s approved for acute VVC [vulvovaginal candidiasis]. They’ve submitted their SNDA [supplemental new drug application] for recurrent VVC by phase 3 clinical trials, with a PDUFA [Prescription Drug User Fee Act] date in November. I’d love to get your take on this newer medication and how you feel this 1 may fit in to the overall treatment paradigm.
Jack D. Sobel, MD: Before we go on, we need to mention that fluconazole isn’t used in pregnant women.
Michael L. Krychman, MD: Correct.
Jack D. Sobel, MD: We also don’t give fluconazole to women who are trying to become pregnant. For example, if a patient is 20 to 23 years old and would like to start a family, but they have recurrent candidal vaginitis and have been on fluconazole maintenance therapy once a week for the last 2 weeks, months, or years, depending on the clinical scenario. They’d like to start having a baby. But we warn her that the risk of fluconazole in pregnancy is greatest in women who aren’t aware that they’re pregnant. It’s the inadvertent administration of fluconazole to a pregnant woman, and the risks are greatest in the first trimester. We have to warn women who are doing wonderfully well on fluconazole about avoiding it if they’re trying to become pregnant. That’s not such an easy thing. Of course, oteseconazole, ibrexafungerp, and fluconazole also shouldn’t be used in pregnancy. Managing pregnant women with recurrent VVC requires going back 30, 40 years, when we used repeated courses of topical agents, either nystatin or clotrimazole, during pregnancy. That was long, but I wanted to clarify that none of these 3 drugs is to be used during pregnancy.
Michael L. Krychman, MD: I appreciate that. People are pushing the envelope and forgetting the basics. We have to throw in the concept of adequate contraception if they’re trying to get pregnant or are pregnant. That’s an important point.
Jack D. Sobel, MD: Oteseconazole is contraindicated in pregnancy, as are fluconazole and ibrexafungerp, but it’s also not approved. It shouldn’t be used by a woman with reproductive ability or who had their tubes tied or a hysterectomy or who is postmenopausal. At this stage, they shouldn’t be given oteseconazole. That may change as more data arrive, but for the next few months, these are some of the limitations.
The FDA is likely to approve ibrexafungerp. It’s given once a month for 6 months. As with many new drugs, like oteseconazole and ibrexafungerp, physicians are going to learn how to use these drugs. They’re going to learn how to master these drugs. There’s never been a study with ibrexafungerp given once a month. If it was given once a week, would it be better? They haven’t done a study comparing 1 week with 1 month. We don’t know the optimal dosage for the maintenance. It will probably be approved at once a month, but maybe it would be better at once a week.
Likewise, it’s going to get approval for 6 months’ use in recurrent candidal vaginitis. Would it be as effective if you gave it for only 4 months? Those dosage-duration studies haven’t been done. If we have the same discussion in 5 or 10 years, we’ll have a whole different perspective with these new agents based on information that doesn’t exist today.
Michael L. Krychman, MD: We have a lot of unanswered questions.
Jack D. Sobel, MD: There are lots of unanswered questions. In the meantime, I suspect that ibrexafungerp will be an alternative, constitute fluconazole. Regardless of whether it will be used in women, it will definitely be useful for patients allergic to or intolerant of fluconazole. It has some contraindication or resistance to fluconazole. That will immediately make you think of oteseconazole or ibrexafungerp. As we know from our clinical practice, what you prescribe depends not on your science and knowledge of genetics but on what the insurance company makes available.
Transcript Edited for Clarity
Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.