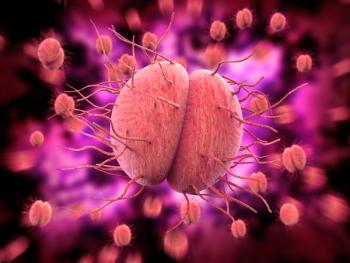
Host immune responses in recurrent vulvovaginal candidiasis
A study published in Frontiers in Immunology indicates that for the prognosis of recurrent vulvovaginal candidiasis (RVVC) and vulvovaginal candidiasis (VVC), the host-immune responses, particularly Th1/2 immunity, may play a vital role.
“Although risk factors of RVVC and VVC have been identified in many studies, antifungal immunological mechanisms are still not fully understood,” wrote the authors.1
The 1-year prospective study, which was conducted at the Jining No. 1 People’s Hospital, a public hospital in Shandong Province, China, enrolled 98 patients clinically diagnosed with gynecological Candida infection.
Overall, 79.59% of patients had VVC and 20.41% had RVVC.
Although the onset age and mean age of the VVC group were younger than the RVVC group, more than 50% of participants in both groups were of reproductive age.
C. albicans accounted for 96.1% and 90% of all strains isolated and collected from VVC and RVVC patients, respectively.
On the other hand, antifungal susceptibility testing found no significant difference in Candida species between RVVC and VVC patients.
However, the serum levels of interferon gamma (IFN-γ), tumor necrosis factor (TNF-α) and interleukin 17F (IL-17F) were significantly lower in the RVVC group compared to the VVC group.
Conversely, IL-4, IL-6 and IL-10 were higher in RVVC patients than VVC patients.
But IL-17A and IL-2 levels were similar for the two groups.
“Given that C. albicans is considered an opportunistic pathogen with a prolonged colonization state in the host before active infection, such a colonization phase could play a vital role in the pathogenesis of idiopathic RVVC,” wrote the authors.
The authors also assessed external risk factors for RVVC and VVC by analyzing medical treatment history, clinical symptoms and any other concurrent infections. They found that antibiotic therapies of azithromycin, clindamycin or cephalosporin, or antifungal metronidazole treatments, highly correlated with candidal vaginitis (P < 0.05).
By contrast, symptomatic factors such as discomfort after sexual activity, redundant prepuce, genital itching, chlamydia and mycoplasma infections had no likely impact on RVVC or VVC (P > 0.05). Medical conditions like gastritis, allergic rhinitis and skin disorders also had no effect on RVVC or VVC (P > 0.05).
In addition, previous use of antifungal agents like nysfungin and clotrimazole for previous episode(s) of RVVC or VVC had no apparent impact on recurrence (P > 0.05).
But family history accounted for 5% and 5.3% of cases, respectively P > 0.05).
The distribution of Candida species does not explain the clinical difference between RVVC and VVC, according to the authors.
Among the vaginal specimens, 98 out of 170 Candida isolates were identified as C. albicans, C. glabrata or C. tropicalis.
Based on the sequencing results of 98 isolates, 94.9% of isolates were C. albicans, 3.1% were C. glabrata and 2% were C. tropicalis (2%).
In 78 strains isolated from the VVC group, 96.10% were C. albicans, and the remainder of the strains were either C. glabrata or C. tropicalis.
Of 20 isolates from the RVVC group, C. albicans represented 90% of isolates, while C. glabrata and C. tropicalis each accounted for 5%.
Although C. glabrata was 100% susceptible to fluconazole and micafungin, the minimum inhibitory concentration (MIC 50/90) of C. glabrata isolates to other drugs, except amphotericin B and terbinafine, was higher than for C. albicans.
Reference
- Ge G. Yang Z, Li D. Distinct host immune responses in recurrent vulvovaginal candidiasis and vulvovaginal candidiasis. Front. Immunol. Published online July 28, 2022. doi:org/10/3389/fimmu.2022.959740
Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.