Pregnancy outcomes affected by aerobic vaginitis
Aerobic vaginitis (AV) in pregnant Vietnamese women correlated with a higher risk of puerperal sepsis and negative pregnancy outcomes.
Anh Thi Chau Nguyen, PhD, of the department of microbiology at Hue University of Medicine and Pharmacy in Hue, Vietnam and colleagues conducted the study, which was published in the journal BMC Pregnancy and Childbirth.1
Symptoms of AV, which can vary in severity and can last for a long time, include yellow or yellow-green pus-like discharge, redness of the vaginal opening and the vagina, a rotten odor, painful intercourse. Severe cases can include ecchymotic bleeding points and erosions, researchers said.
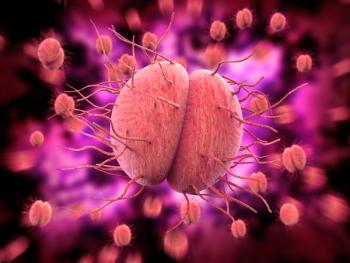
The hallmark of AV is the existence of facultative and aerobic bacteria such as S. aureus, E. coli, E. faecalis, S. agalactiae, and coagulase-negative staphylococci. “AV is described as a depletion of the Lactobacillus microbiota and an increase in aerobic bacteria derived mainly from the gastrointestinal tract, accompanied by inflammatory markers and deficient epithelial maturation,” the authors wrote.
Researchers performed a cross-sectional descriptive study that examined 323 pregnant women during routine prenatal care visits at Hue University Hospital in Hue, Vietnam between July 2018 and January 2019. Study participants had a mean age of 28.3 years, and researchers said most of the women had secondary or above levels of education. Most were employed as public servants or were housewives. Almost all study participants were married, with only 0.6% reporting their status as single. None of the women had fetuses with abnormalities.
Women who had been treated for reproductive infections or who had used antibiotics within the last week for some other type of infection, a previous diagnosis of a ruptured membrane, or douching before or during the collection of the specimen were excluded from the study. Women who experienced antepartum hemorrhaging were also not included.
Nguyen and colleagues examined vaginal specimens obtained during the third trimester using 2 sterile cotton swabs to collect vaginal fluid. One swab was analyzed using Gram-stained slide smear, and the second was frozen in cryotube for culturing at a lab in Estonia. Researchers used the Donders scoring system and cultured the swabs for predominant bacteria identification. The authors followed the women’s pregnancies to term and recorded outcomes for both infants and mothers.
Over 15% of the women had AV in the third trimester, researchers reported. Eighty-four percent had light AV, while 16% had moderate AV. Of positive samples, S. agalactiae (6%), Enterococcus sp (4%), and S. aureus (4%) were the most common microorganisms. Third trimester AV correlated with an increased risk of puerperal sepsis (OR 8.65, 95% CI: 1.41—53.16, p=0.020) and researchers said there was an increased risk of neonatal infections, although this was not statistically significant.
“Previous studies have revealed that AV can be related to different pregnancy complications like chorioamnionitis, fetal infection, premature birth,” researchers said, in addition to premature rupture of membranes, preterm premature rupture of membranes, and neonatal infections. Nguyen and colleagues said that less data is available regarding postpartum infections and that complications of AV are similar to bacterial vaginosis.
Of women in the study, 6% had puerperal sepsis, and the authors emphasized that women with AV have a 9-fold risk of postpartum infection. Nguyen and colleagues stressed that postpartum infections worldwide are 1 of the top 5 causes of maternal death, and cause 10 to 15% of deaths in the postpartum period. 75,000 maternal deaths yearly are attributed to puerperal sepsis, the authors explained.
“AV in pregnant women is significantly associated with an increased risk of postpartum infections and therefore needs to be diagnosed and treated before delivery,” Nguyen and colleagues concluded.
Lubna Mohammed, MBBS, Internal Medicine at the California Institute of Behavioral Neurosciences & Psychology, who was not associated with the study, told Contemporary OB/GYN® that the most important takeaway from this study for providers in practice is the importance of diagnosing AV before delivery as it is related to a higher risk of developing puerperal sepsis and other complications.
“For next steps, researchers should study the prevalence of AV in pregnant women belonging to all demographical populations so that a vigilant eye can be kept to diagnose and treat it, as the current study only concentrates on the Vietnamese population,” she said in the interview.
Mohammed added that even though the third trimester of pregnancy starts at 28 weeks, most of the samples in this study were collected after 37 weeks. “Diagnosing AV from the beginning of the third trimester can be considered by ob-gyn provider audience and the outcome of early diagnosis can be studied,” she said.
Reference
- Nguyen ATC, Le Nguyen NT, Hoang TTA, et al. Aerobic vaginitis in the third trimester and its impact on pregnancy outcomes. BMC Pregnancy Childbirth. 2022;22(1):432. Published 2022 May 24. doi:10.1186/s12884-022-04761-5
Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.