Tetrazole oteseconazole (VT-1161) may be used as an alternative therapeutic method against Candida albicans, according to a recent study published in BioMedicines.
Takeaways
- The study suggests that tetrazole oteseconazole, a new generation fungal CYP51 inhibitor, exhibits in vitro activity against Candida albicans, making it a potential alternative treatment for recurrent vulvovaginal candidiasis (VVC).
- With increasing resistance to fluconazole, particularly in biofilm-forming Candida strains, there is a critical need for new therapeutic options to combat recurrent VVC effectively.
- The study involved challenging Candida biofilms with amphotericin B to identify persister cells, which play a role in recurrent infections, and evaluating tetrazole oteseconazole's effectiveness against these cells.
- The efficacy of tetrazole oteseconazole in eradicating Candida biofilms was dose-dependent, with higher concentrations associated with greater eradication rates for both primary and secondary biofilms.
- In addition to its efficacy against Candida isolates, tetrazole oteseconazole showed positive safety and efficacy data in vitro, with larva survival rates up to 70%, suggesting its potential as a safe treatment option for patients with recurrent candidiasis.
C. albicans is responsible for over 50% of candidemia cases such as vulvovaginal candidiasis (VVC). VVC infection at least once in an individual’s lifetime is reported in approximately 70% of women, with risk factors including pregnancy, frequent antibiotic use, oral contraceptives, gestational diabetes mellitus, and lackluster treatment.
Recurrent VVC is often treated using fluconazole, but data has indicated increased resistance to this treatment. This resistance is often linked to the ability of Candida to create biofilms on biotic and antibiotic surfaces which reduces antifungal penetration. Therefore, new therapeutic options are needed.
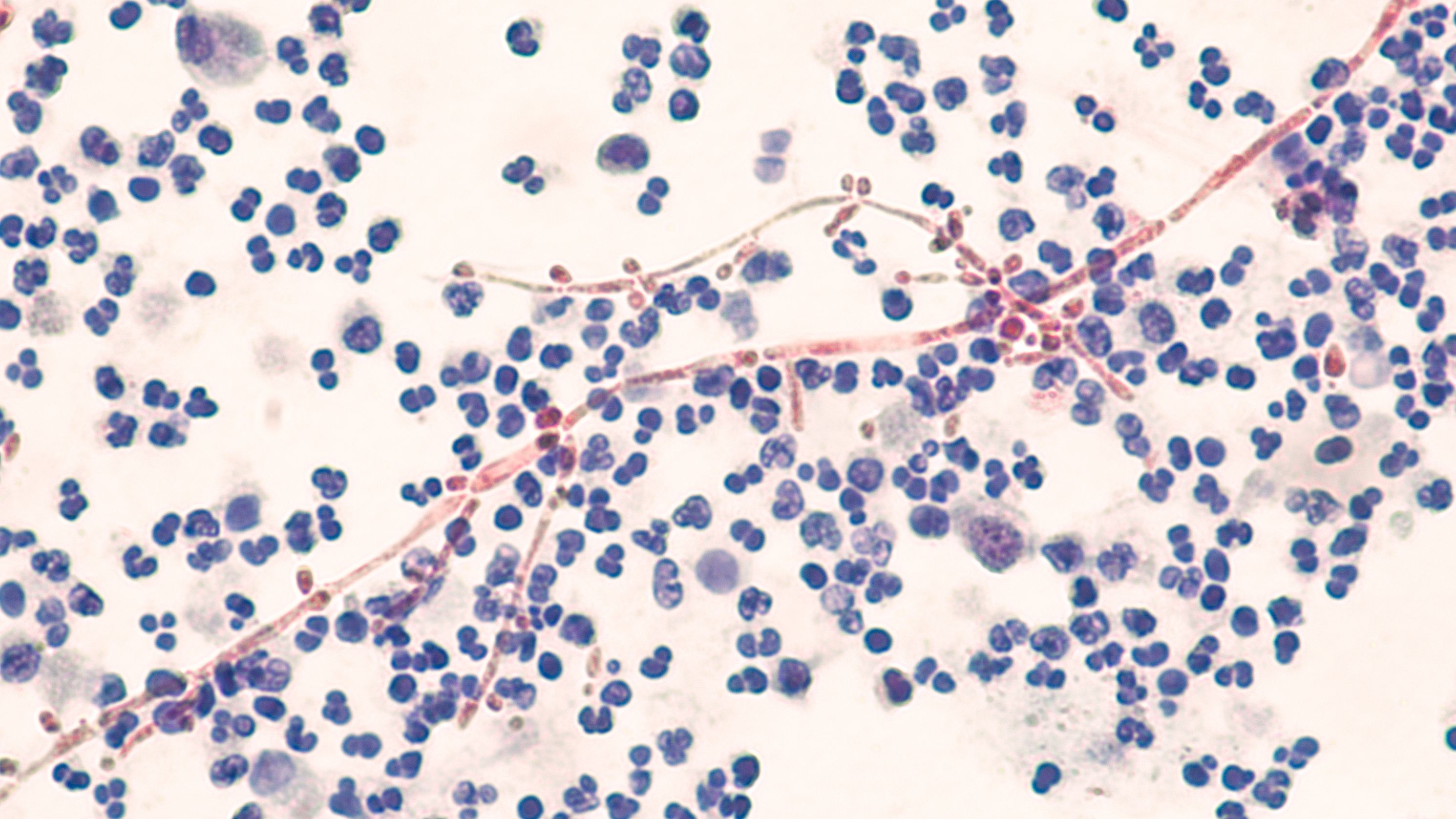
Tetrazole oteseconazole, representing a new generation of fungal CYP51 inhibitors with high fungal specificity, has displayed in vitro activity against C. albicans. Investigators conducted a study to further investigate its ability to eradicate a biofilm developed by a C. albicans vaginal fluconazole-resistant isolate.
The Candida isolate was stored at -80 ◦C and maintained on rose bengal agar (RB, Sigma-Aldrich, St. Louis, MO, USA). Investigators performed dilution in phosphate-buffered saline (PBS, Oxoid Ltd., Basingstoke, UK) to identify viable Candida cells.
Persister cells were identified in C. albicans biofilm by challenging the biofilm with amphotericin B (Amph B) buffered to pH 7 with 0.165 M morpholinopropanesulfonic acid (MOPS, Sigma-Aldrich Co., St. Louis, MO, USA). Concentrations were measured between 5 and 200 µg mL−1.
Biofilm was then washed with PBS, then scraped and vortexed for 30 seconds. The number of surviving cells was expressed as log colony-forming units (CFU) per well to quantify persisters. The cells that survived Amph B treatment were used to create a secondary biofilm (B2). CFU assay was utilized to estimate B2 recovery every 48 hours.
For 24 hours, B2 was exposed to either 0.5, 1, or 2 µg mL−1 of tetrazole oteseconazole. This was done to assess the drug’s eradication activity, measured as % = (OD570 control − OD570 sample/OD570 control) × 100. OD570 control and OD570 sample were based on the untreated and treated biofilm, respectively.
The adhesion ability of planktonic and B2-derived cells was also evaluated to identify the effectiveness of tetrazole oteseconazole in displacing adhered Candida cells. Finally, G. mellonella survival assays were conducted to evaluate the drug’s antifungal effect in utero.
C. albicans had a minimum inhibitory concentration (MIC) of 2 µg mL−1 for Amph B and tetrazole oteseconazole, indicating a strong biofilm production ability in utero. Amph B was able to kill fungal cells in all stages of growth, making it one of the most effective antifungal agents. Because of this, C. albicans biofilm was challenged using Amph B concentrations up to 100 X MIC.
Approximately 0.001% of the mature biofilm population was persister, reinforcing the idea of C. albicans vaginal isolate persister cells being present in biofilms. Over time, the number of living cells in B2 increased over time, reaching the value of the primary biofilm (B1) in 3 days.
An association was reported between the dose of the drug administered and the eradication of both the primary and secondary biofilms. Sub-MIC concentrations of 1 μg mL−1 were associated with a 70% eradication of B1 and 55% eradication of B2. However, a reduced concentration of 0.5 μg mL−1 was associated with 40% eradication for both biofilms.
Tetrazole oteseconazole administration was also associated with displacement of Candida cells from human keratinocyte (HaCaT). A partial decrease in adherence was reported for a dosage of 0.5 μg mL−1, while concentrations of 1 and 2 μg mL−1 were associated with a displacement of almost 90%. In vitro safety and efficacy data were also positive, with larva survival up to 70% reported.
These results indicated tetrazole oteseconazole is effective against C. albicans isolates. Investigators concluded it could be considered as an alternative therapeutic option for patients with recurrent candidiasis.
Reference
Sinoca M, Maione A, Gambino E, et al. A preliminary evaluation on the antifungal efficacy of VT-1161 against persister Candida albicans cells in vulvovaginal candidiasis. Biomedicines. 2024;12(2):389. doi:10.3390/biomedicines12020389