- Vol 67 No 11
- Volume 67
- Issue 11
Phase 3 data show oral oteseconazole successful for treating vulvovaginal candidiasis and infections
The medication also performed comparably to vulvovaginal candidiasis (VVC) standard-of-care fluconazole for treating acute VVC infection.
For the treatment of recurrent vulvovaginal candidiasis (RVVC), oral oteseconazole (Vivjoa; MYCOVIA) was found safe and highly efficacious in treating and preventing the infection, according to phase 3 data published in the American Journal of Obstetrics and Gynecology.1
The medication also performed comparably to vulvovaginal candidiasis (VVC) standard-of-care fluconazole for treating acute VVC infection.
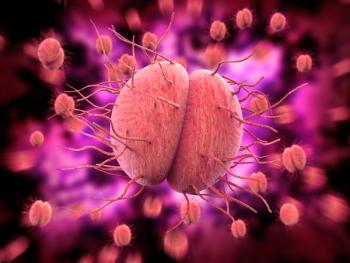
Oteseconazole is a novel oral selective inhibitor of fungal lanosterol demethylase: sterol 14α-demethylase cytochrome P450, an enzyme required for fungal growth.
The study assessed the efficacy and safety of oral oteseconazole in preventing recurrent culture verified acute VVC episodes up to 50 weeks, as well as comparing the drug to fluconazole in treating the presenting acute VVC episode.
A total of 219 women and postmenarcheal girls, aged 12 years and older, with a history of RVVC were enrolled at 38 U.S. clinical sites.
Patients were randomly assigned in a 2:1 ratio to the oteseconazole group or the fluconazole/placebo group.
In an induction phase, patients in the oteseconazole group received 600 mg of oteseconazole (four 150-mg capsules) on day 1; 450 mg of oteseconazole (three 150-mg capsules) on day 2; and a single placebo capsule on days 4 and 7.
By comparison, patients in the fluconazole/placebo group received 3 150-mg capsules of overencapsulated fluconazole, each capsule spaced 72 hours apart over 7 days. The group also took additional placebo capsules to match the number of capsules administered to the oteseconazole group, to maintain blinding.
Patients returned roughly 2 weeks after their first induction phase dose for the investigator to determine whether the presenting acute VVC infection had resolved, which was defined as a signs and symptoms score of less than 3.
Patients assigned to the oteseconazole group, whose acute VVC had resolved, then entered a maintenance phase of 11 weeks, during which time they received oteseconazole 150 mg once weekly, whereas patients in the fluconazole/placebo group whose acute VVC infection had resolved received once-weekly placebo.
Patients were followed for an additional 37 weeks.
For the induction phase, oteseconazole was found comparable to fluconazole in the percentage of patients in the intent-to-treat population with resolved acute VVC infection at the 2-week test-of-cure visit: 93.2% vs. 95.8%, respectively.
For the maintenance phase, though, oteseconazole was superior to placebo in the percentage of patients in the intent-to-treat population with at least one culture-verified acute VVC episode through week 50: 5.1% vs. 42.2%, respectively (P < 0.001).
Treatment-emergent adverse event rates were similar between patients who received oteseconazole in the induction and maintenance phases and patients who received fluconazole in the induction phase and placebo in the maintenance phase: 54% vs. 64%, respectively.
Most of these adverse events were mild or moderate, with only 3.4% graded as severe or higher in the oteseconazole group and 4.2% in the fluconazole/placebo group.
“Oteseconazole efficacy, duration of efficacy, and favorable safety profile, together with its broad spectrum of antifungal activity against many Candida species, including fluconazole-resistant strains, proved that this drug could become a novel option to treat and prevent recurrent episodes of VVC,” concluded the authors.
Reference
Martens MG, Maximos B, Degenhardt T, et al. Phase 3 study evaluating the safety and efficacy of oteseconazole in the treatment of recurrent vulvovaginal candidiasis and acute vulvovaginal candidiasis infections. Am J Obstet Gynecol. Published online July 19, 2022. doi:10.1016/j.ajog.2022.07.023
Articles in this issue
about 3 years ago
Bowel injury after operative hysteroscopyabout 3 years ago
Readers React: Neutral language has adverse effectsover 3 years ago
EMIGS: A new standard of careover 3 years ago
Endometrial ablation in the office settingover 3 years ago
Fundraising for early-stage start-upsover 3 years ago
Cheerleading and game plansover 3 years ago
Virtual IUD placement training improves clinician confidenceNewsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.