- Vol 67 No 12
- Volume 67
- Issue 12
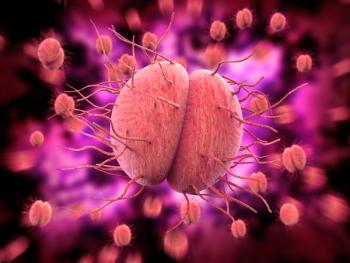
Prevalence of Candida species with IUD placement
Three months after copper intrauterine device (IUD) insertion, nearly 1/3 of women were diagnosed with vulvovaginal candidiasis, compared to nearly 25% of women who received a hormonal IUD, according to a prospective study published in the journal Cellular and Molecular Biology.
The 2 groups differed significantly in the prevalence of the species of candidiasis.
The longitudinal study comprised 160 women who volunteered for IUD use and were referred to health centers in China. Cervicovaginal swabs were taken from the women, none of whom showed signs of vaginal infection during the vaginal examination.
Patients were then divided equally into 2 groups. The first group (n=80) received the Mona Lisa NT Cu380 copper IUD and the second group (n=80) received the Mirena hormonal IUD.
Patients did not use antibiotics or antifungal drugs at least 2 weeks prior and 3 months after IUD placement.
Samples were cultured in a Sabouraud dextrose agar (SDA) medium. The milky yeast colony was then transferred to chromium agar culture medium. Fungal species were differentiated by dyeing, with P <0.05 considered significant.
In total, 70 women in the copper IUD group and 61 women in the hormonal IUD group completed the study. Overall, 29.57% of women who received the copper IUD were diagnosed with candidiasis 3 months post-insertion, compared to 22.95% of women who received the hormonal IUD.
There was a significant difference, though, in the prevalence of individual species between the 2 groups (P = 0.031).
In the copper IUD group, 14 of the 21 patients with Candida species had albicans, 5 patients had glabrata and 2 patients had parapsilosis.
By contrast, in the hormonal IUD group, 10 of the 14 patients with Candida species had albicans, 3 patients had glabrata and 1 patient had parapsilosis.
The significant increase in the incidence of vulvovaginal candidiasis within 3 months after IUD placement has been reported in previous studies and is due to changes in the microbial flora of the reproductive system.
An inflammatory reaction and cellular changes are caused by the foreign body of the IUD in the uterus and the constant secretion of copper or hormones. This leads to changes in the dominant microflora and escalating Candida colonization.
The increase in glabrata species is noteworthy after IUD placement, according to the authors, because it can create drug resistance andprompt recurrent vulvovaginal candidiasis.
“Because Candida albicans is found in the vaginal microflora of 30% to 80% of asymptomatic women, the decision to treat asymptomatic cases requires further study and testing,” wrote the authors.
Candida chromium agar differential culture medium is easy to use, reproducible and cost-effective, according to the authors.
However, in cases like recurrent or complicated vulvovaginal candidiasis, where accurate diagnosis is needed for successful treatment, sensitive and precise molecular methods, such as polymerase chain reaction (PCR), is advised.
The authors also advocate further studies with wider dimensions and longer follow-up periods to confirm the findings of the current study.
Reference
Wei T, Wang H, Wen B. Comparison of copper IUDs and hormonal IUDs in prevalence of Candida species in cervicovaginal smears. Cell Mol Biol. 2022 Jan 2;67(4):130-134.
Articles in this issue
about 3 years ago
The importance of huddlesabout 3 years ago
Surgical treatments for endometriosisabout 3 years ago
Uterine anomalies in pregnancyabout 3 years ago
Leadership in the new realityNewsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.