- Vol 67 No 7
- Volume 67
- Issue 7
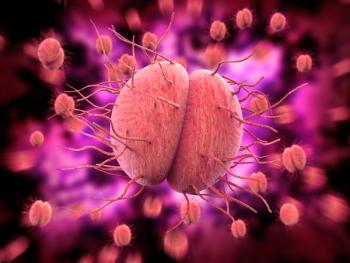
Vulvodynia not associated with vulvovaginal candidiasis
Not only does vulvodynia impact a woman’s sexual and psychological health, but it also places significant financial burden on those seeking treatment.
Researchers estimate that as many as 15% of women in the United States suffer from vulvodynia, or persistent vulvar pain with no clear etiology.1 Not only does vulvodynia impact a woman’s sexual and psychological health, but it also places significant financial burden on those seeking treatment.
In the US, the estimated cost per treatment course is around $9600, and focuses mostly on symptom management.2 Researchers have conducted numerous studies in search of a potential etiology, with emerging interest in a potential link between vulvodynia and vulvovaginal candida infection (VVC). Those findings, however, lacked laboratory confirmation of candida. A study in Women’s Health Reports investigated further.
Researchers conducted a retrospective analysis to determine whether laboratory confirmed VVC was associated with vulvodynia diagnosis. They used data from patients’ electronic health records, which were originally obtained from 2017 to 2020 during visits for routine and specialty vulvar care at an academic women’s health practice in central Texas.
The clinic utilized the Q-Tip test and reports of persistent vulvar pain without identifiable etiology to establish vulvodynia diagnosis. Providers collected an agar-based genital yeast culture from all patients with vulvar pain as part of the initial work-up and conducted polymerase chain reaction (PCR) testing in patients who met the criteria of the 2015 International Society for the Study of Vulvovaginal Disease criteria.
Patients completed questionnaires at the time of intake, including the Vulvar Pain Functional Questionnaire, Female Sexual Function Index, Generalized Anxiety Disorder, and Patient Health Questionnaire.
The study included a total of 242 women, 64 (26.4%) of whom were diagnosed with vulvodynia, and 178 (73.6%) were not. Researchers did not find a difference in the number of women
with confirmed yeast infections with or without a diagnosis of vulvodynia (75% vs. 70%, p = 0.718). Nearly 1/3 of women in the study had confirmed yeast infections (29%) and 27 (11%) received PCR testing. According to PCR results, C. albicans accounted for 20 (75%) infections and the other 7 (25%) were nonalbicans.
A total of 73% of participants self-identified as white and 30% identified as Hispanic. The median body mass index (BMI) was 26.7kg/m2 and was significantly lower in patients with vulvodynia (t = 2.65, df = 120, p = 0.009). The findings also showed that 61% of the patient population had anxiety and were more likely to have vulvodynia (t = 2.65, df = 120, p = 0.009; 78% vs 55%, p = 0.002).
The findings did not include a connection between VVC and vulvodynia. The reason for this, the authors speculate, is largely attributed to the prior studies’ reliance on self-reported data. Relying on reported history without laboratory results, according to the authors, could contribute to over-reporting in patients with increased vulvar sensitivity.
However, the findings did include an association between vulvodynia and low BMI and anxiety. To improve on generalizability, the authors highlighted a need to include more women of color with vulvodynia in future studies.
References
- Domenici. Vulvodynia: current opinion and treatment strategies. Minerva ginecologica. 2016;68(6). Accessed April 7, 2022. https://pubmed.ncbi.nlm.nih.gov/26126068/
- Lua LL, Hollette Y, Parm P, Allenback G, Dandolu V. Current practice patterns for management of vulvodynia in the United States. Archives of Gynecology and Obstetrics. 2016;295(3):669-674. doi:10.1007/s00404-016-4272-x
Articles in this issue
over 3 years ago
Beware of “forever chemicals”over 3 years ago
Demystifying AVMsover 3 years ago
A missed opportunity: annual screenings are essentialalmost 4 years ago
Twice weekly maintenance therapy ideal for recurrent yeast infectionsNewsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.