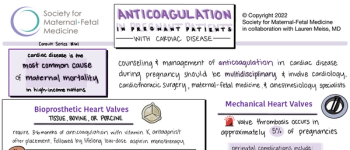
View the latest recommendations from the Society for Maternal-Fetal Medicine on anticoagulation in pregnant patients with cardiac disease.

The Society for Maternal-Fetal Medicine supports the clinical practice of maternal-fetal medicine by providing education, promoting research, and engaging in advocacy to optimize the health of high-risk pregnant women and their babies.
View the latest recommendations from the Society for Maternal-Fetal Medicine on anticoagulation in pregnant patients with cardiac disease.

In this consult series, experts from SMFM discuss the evaluation and management of soft ultrasound markers for aneuploidy.
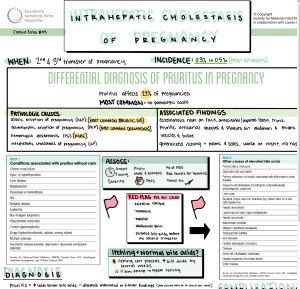
From SMFM, a visual summary of Consult #60.

This Consult discusses the management of pregnancies achieved with in vitro fertilization and provides recommendations based on the available evidence.
This Consult has been endorsed by the American College of Obstetricians and Gynecologists (ACOG) and replaces the Society for Maternal-Fetal Medicine's (SMFM) Statement #4, Implementation of the use of antenatal corticosteroids in the late preterm birth period in women at risk for preterm delivery, August 2016.

Get the Facts. Get Vaccinated.
The COVID-19 global pandemic has broad implications for obstetrical care and perinatal outcomes. As we approach the 2-year mark into an unprecedented international pandemic, this review presents the progress and opportunities for research related to COVID-19 and pregnancy.

SMFM supports the new NIH COVID-19 Treatment guidelines.

The Society for Maternal-Fetal Medicine has published an update for provider considerations for COVID-19 vaccine counseling with pregnant or lactating patients.

Pregnant? Thinking about pregnancy? Recently pregnant? Check out the top 5 reasons to get the COVID-19 vaccine from the Society for Maternal-Fetal Medicine.

Patients Desiring Immediate Postpartum Sterilization Should Not Be Required to Wait 30 Days.

SMFM Consult Series #56: Hepatitis C in pregnancy: updated screening, treatment, and management guidelines.

Download a visual summary of SMFM Consult Series #56: Hepatitis C in pregnancy: updated guidelines

Registration is now open for the Society for Maternal-Fetal Medicine's (SMFM) 42nd Annual Pregnancy Meeting, to be held from January 31 to February 5, 2022, at the Gaylord Palms Resort and Convention Center near Orlando, Florida.
The path to transformational leadership.
The course will cover a range of high-risk OB topics with an emphasis on clinical management, in the form of lectures, case presentations, panel discussions and audience participation.
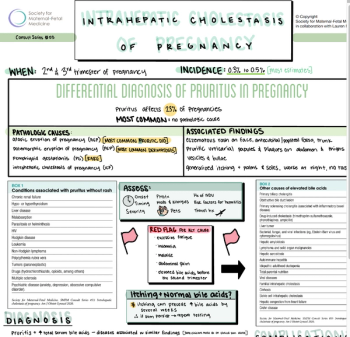
Refer to this visual summary from SMFM wherever you practice.

Intrahepatic cholestasis of pregnancy (ICP) occurs in the second and third trimesters of pregnancy and is characterized by pruritus and elevated serum bile acid concentrations.
This year’s annual meeting of the Society for Maternal-Fetal Medicine (SMFM) will go down in history as one to remember.

A challenge in the prenatal management of FGR is differentiating the constitutionally small fetus with a normal neonatal outcome from one who is pathologically growth restricted and at risk for postnatal complications.

The Society for Maternal-Fetal Medicine’s (SMFM) 2021 Annual Pregnancy Meeting will be held virtually throughout the month of January, with core meeting activities taking place Jan. 25-30. SMFM’s President, Judette Louis, MD, MPH, and Program Committee Chair, Cynthia Gyamfi-Bannerman, MD, MSc, tell readers what they can expect in the new online format.

The risk of venous thromboembolism is particularly high during the postpartum period and especially following cesarean delivery.

Little evidence supports the routine use of activity restriction for preterm birth and other obstetric conditions, and some data indicate adverse impact on obstetric outcomes.

Cesarean scar pregnancy (CSP) is a complication in which an early pregnancy implants in the scar from a prior cesarean delivery. Incidence and recognition of this condition appear to have increased over the past two decades, perhaps due to high worldwide cesarean delivery rates. The clinical presentation is variable, and many women are asymptomatic at presentation. CSP can be difficult to diagnose in a timely fashion. Ultrasound is the primary imaging modality for CSP diagnosis. Expectantly managed CSP is associated with high rates of severe maternal morbidity such as hemorrhage, placenta accreta spectrum (PAS), and uterine rupture. Given these substantial risks, pregnancy termination is recommended after CSP diagnosis. Several surgical and medical treatments have been described for this disorder, but at this time, optimal management remains uncertain.


Cesarean scar pregnancy (CSP) is a complication in which an early pregnancy implants in the scar from a prior cesarean delivery. Incidence and recognition of this condition appear to have increased over the past two decades, perhaps due to high worldwide cesarean delivery rates. The clinical presentation is variable, and many women are asymptomatic at presentation. CSP can be difficult to diagnose in a timely fashion. Ultrasound is the primary imaging modality for CSP diagnosis. Expectantly managed CSP is associated with high rates of severe maternal morbidity such as hemorrhage, placenta accreta spectrum (PAS), and uterine rupture. Given these substantial risks, pregnancy termination is recommended after CSP diagnosis. Several surgical and medical treatments have been described for this disorder, but at this time, optimal management remains uncertain.

Among women who died from sepsis, a majority had a delay in care and a delay in escalation of care.

This summary of SMFM Consult Series #46 reviews major considerations in evaluation and management of polyhydramnios.

Ventriculomegaly, or dilation of the fetal cerebral ventricles, is a relatively common finding on prenatal ultrasound. This summary of SMFM Consult Series #45 reviews key points for diagnosis, evaluation, and management of mild fetal ventriculomegaly.

In the United States, 1% to 2.5% of pregnant women are infected with hepatitis C virus (HCV), which carries an approximately 5% risk of transmission from mother to infant. HCV can be transmitted to an infant in utero or during the peripartum period.
Published: March 15th 2021 | Updated:

Published: January 20th 2022 | Updated:

Published: June 11th 2020 | Updated:

Published: January 4th 2021 | Updated:
Published: July 8th 2021 | Updated:

Published: March 12th 2021 | Updated: