- Vol 64 No 9
- Volume 64
- Issue 9
Gadolinium-based contrast in breast MRI: What ob/gyns need to know
Concerns have been raised about the safety of GBCA. Experts review the latest data to support counseling of patients who may have repeated exposure.
Magnetic resonance imaging (MRI) uses magnetic fields to provide detailed anatomic images that reflect distribution and magnetic properties of tissues (specifically of hydrogen nuclei in water and fat) to aid in diagnosis of many pathologic conditions. Gadolinium-based intravenous contrast agents (GBCA) provide additional information based on signal intensity changes after GBCA administration. GBCA are used in approximately 45% of MRI exams in the United States. In the 30 years since the first GBCA was introduced into clinical practice, almost a half billion enhanced MRI studies have been performed worldwide. In the field of gynecology, MRI is widely used to enhance detection of early breast cancers in women at elevated risk, or to better delineate complex pelvic anatomy in the setting of prior pelvic surgery, severe endometriosis, distorting fibroids, cervical, uterine cancer or ovarian cancer.
A recent concern with use of GBCA surfaced in 2014, when the link between permanent high T1 signal in the dentate nucleus and globus pallidus of the brain and repeated prior GBCA exposure was identified.1 Post-mortem analysis of these deep brain structures confirmed that gadolinium deposition in the brain of patients who had GBCA-enhanced MRI of any part of the body. Specifically, higher signal intensities were seen in patients who had undergone at least six contrast-enhanced MRI examinations compared to patients who had undergone only non-contrast MRI. Case reports in children noted the same pattern of gadolinium deposition as that seen in adult patients following GBCA.2 Industry-sponsored studies in rats serially exposed to GBCA found progressively higher signal intensity on imaging, which correlated with post-mortem gadolinium concentrations in the brain.3 Notably, at the time of this writing, no human or animal data have shown any association between GBCA exposure and neurologic toxicity or neurological symptoms related to gadolinium deposition in the dentate nucleus of globus pallidus.4 Ob/gyns need to be aware of the current data about gadolinium-based contrast and the potential implications of its use when they order MRI for their patients.
Consensus guidelines on GBCA
In response to the reports of gadolinium deposition in the brain of GBCA-exposed individuals, the US Food and Drug Administration (
Gulani and colleagues, on behalf of the International Society for Magnetic Resonance in Medicine (
Implications for MRI utilization in gynecology
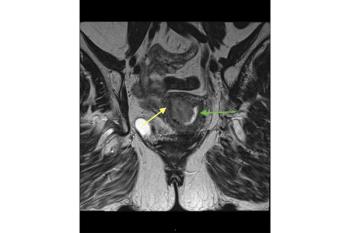
MRI imaging of the pelvis is indicated to further characterize masses seen on computed tomography (CT) or ultrasound. An MRI without contrast offers sensitivity comparable to CT with contrast and superior specificity in diagnosis of adnexal malignancy following an indeterminate ultrasound.9 MRI provides better assessment of soft tissue structures and improved localization of pelvic masses, which is useful to discriminate between ovarian and uterine pathology. T2-weighted imaging is helpful in determining whether the lesion is a unilocular cyst, mixed solid and cystic, or homogeneously solid. T1-weighted imaging without and with fat saturation allows for detection of adnexal lesions containing macroscopic fat. Fat-saturated T1-weighted imaging is useful for identifying ovarian endometriomas, extraovarian endometriosis, and other lesions with blood degradation products, such as hemorrhagic cysts.10-12 Adding contrast may allow better discrimination between benign and malignant pathology due to the kinetics of contrast enhancement and washout, although its use may vary by institutional MRI protocol.
The incremental additional clinical information that is gained with use of GBCA in MRI evaluation of variant pelvic anatomy and suspected benign pathology is small. Adding GBCA has been shown to improve evaluation of myometrial invasion from endometrial carcinoma13 and identification of the correct primary tumor when there are multiple sites of biopsy-proven uterine adenocarcinoma.14 Contrast may also be useful in identifying vulvar cancers and occult inguinal metastases15 and it has shown to be useful in identifying neoplastic nodules within complex adnexal lesions and distinguishing endometriosis from pelvic inflammatory disease.16,17
Breast cancer screening in high-risk women
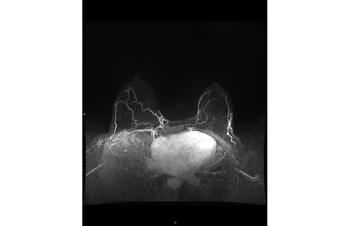
Intensive breast cancer surveillance is advised for women at the highest risk of breast cancer. Women with inherited genetic susceptibility due to BRCA and other less well-known germline mutations (CHEK2, ATM, PALB2), family history, prior chest radiation (cumulative dose > 10 Gy before age 30), or calculated lifetime risk of breast cancer exceeding 20% or more are advised to start breast cancer screening between ages 25 and 30.18,19 While mammography remains the gold standard for breast cancer screening in the general population, it has been less successful in detection of early, curable cancers in higher-than-average-risk patients. Prospective studies of annual mammography in BRCA-positive women showed an interval cancer rate of 35% to 50% and the majority of invasive cancers were > 1 cm and 20% to 56% of them had lymph node involvement.20 Some factors cited to explain the poorer detection of BRCA-associated breast cancer may relate to the confounding effect of breast density, which is more common in younger women. Mammography relies upon abnormal tissue density, tissue distortion, and calcifications to identify breast cancers. BRCA1-associated breast cancers tend to be less mammographically detectable than sporadic breast cancers, which has been attributed to their distinctive histologic growth patterns, such as pushing borders, the relative absence of associated ductal carcinoma in situ, and high cellularity.21
In observational studies, adding contrast-enhanced MRI to annual mammography in BRCA mutation carriers significantly improved detection of early, treatable breast cancers with a combined sensitivity of 94% compared to 39% with mammography alone.18,22,23 MRI provides a functional assessment of breast tissue. Contrast- enhanced MRI can detect microvascular changes and peritumoral inflammation as the contrast accumulates rapidly, and is then washed out rapidly, in more vascular tumors compared to benign breast tissue. Consequently, annual contrast-based MRI has been incorporated into breast cancer surveillance guidelines for women at the highest risk of breast cancer.24
There has been no change to the recommendation of annual breast MRI by the
Some high-volume centers enriched with populations of BRCA mutation carriers have amended the recommended surveillance for women at high risk of breast cancer. Breast ultrasound may be alternated with annual MRI, in addition to annual mammography. Ongoing study of novel strategies to improve the mammogram, such as use of iodinated contrast and breast tomosynthesis, which creates a 3-D image of the breast by stacking multiple 2D mammographic renderings, are underway in women with BRCA mutations. Such advances may allow reduction in cumulative exposure to GBCA in these high-risk women.21
Weighing risks and benefits in women at high risk
While it’s discomforting to consider progressive accumulation of gadolinium in the body over time, the clinical consequences and level of risk associated with GBCA are, as yet, unknown. On the contrary, the consequences of missing an aggressive breast cancer are all too well known. In the absence of an effective non-gadolinium alternative to GBCA, until we have more definitive data on the true risk of gadolinium deposition, we forego surveillance of women at high risk of breast cancer with contrast-enhanced MRI at our peril. Best practice suggests that providers consider the necessity of contrast based upon clinical circumstances, and that macrocyclic rather than linear agents be used when necessary.10 Judicious use of gadolinium, coupled with vigilance in identifying women who might be pregnant, can minimize inadvertent fetal exposure to gadolinium, which is estimated to occur in 1 in 860 pregnancies in the United States.28
Disclosures:
The authors report no potential conflicts of interest with regard to this article.
References:
- Kanda T, Osawa High signal intensity in dentate nucleus on unenhanced T1 weighted MRI images: association with linear versus macrocyclic gadolinium chelate administration. Radiology. 2015;275:803-809.
- Roberts DR, Holden KR. Progressive in of T1 signal intensity in the dentate and nucleus and globus pallidus on unenhanced T1-weighted MR images in the pediatric brain exposed to multiple doses of gadolinium contrast. Brain Devel. 2016;38:331-336.
- Robert P, Lehericy S, Grand S, et al. T1 weighted images hypersignal in the deep cerebellar nuclei after repeated administrations of gadolinium-based contrast agents in healthy rats: difference between linear and macrocyclic agents. Invest Radiol. 2015;50:473-480.
- Terashima KH, Reich DS. Gadolinium deposition: practical guidelines in the face of uncertainty. Lancet Neurol. 2017;16:495-497.
- FDA Safety Communication 5/16/2018 Update https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-gadolinium-based-contrast-agents-gbcas-are-retained-body
- Gulani V, Calamante FG, Shellock FG, et al. Gadolinium deposition in the brain: summary of evidence and recommendations Lancet Neurol. 2017;16:564-570.
- American College of Radiology. Committee on Drugs and Contrast Media. ACR Manual on Contrast Media, Version 10.3. Available at https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf Accessed April 10, 2018.
- European Medicines Agency. PRAC concludes assessment of gadolinium agents used in body scans and recommends regulatory actions, including suspension of for some marketing authorizations. March 2017 Available at
http://www.ema.europa.eu/docs/en_GB/documnent_library/Press_release/2017/03 .
- Kinkel K, Lu Y, Mehdizade A, et al. Indeterminate ovarian mass at US: incremental value of second imaging test for characterization–meta-analysis and Bayesian analysis. Radiology. 2005;236(1):85-94.
- Masch WR, Daye D and Lee SI. MRI imaging for incidental adnexal mass characterization. Magn Reson Imaging Clin N Am. 2017;25(3):521-525.
- Ha HK, Lim YT, Kim HS, et al. Diagnosis of pelvic endometriosis: fat-suppressed T1-weighted vs conventional MR images. AJR Am J Roentgenol. 1994; 163(1):127-131.
- Bazot M, Bharwani N, Huchon C, Kinkel K, et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur Radiol. 2017; 27(7):2765-2775.
- Nougaret S, Horta M, Sala E, Lakhman Y, et al. Endometrial Cancer MRI staging: Updated Guidelines of the European Society of Urogenital Radiology. Eur Radiol. 2019 Feb;29(2):792-805.
- Vargas HA, Akin O, Zheng J, Moskowitz C, et al. The value of MR imaging when the site of uterine cancer origin is uncertain. Radiology. 2011 Mar;258(3):785-792.
- Kataoka MY, Sala E, Baldwin P, et al. The accuracy of magnetic resonance imaging in staging of vulvar cancer: a retrospective multi-centre study. Gynecol Oncol. 2010;117:82-87.
- Suzuki S, Yasumoto M, Matsumoto R, Andoh A. MR findings of ruptured endometrial cyst: comparison with tubo-ovarian abscess. Eur J Radiol. 2012;81(11):3631-3637.
- Tanaka YO, Okada S, Yagi T, et al. MRI of endometriotic cysts in association with ovarian carcinoma. AJR Am J Roentgenol. 2010;194(2):355-361.
- Warner E, Plewes DB, Hill KA, et al. Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA. 2004;292(11):1317-1325.
- Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. J Am Coll Radiol. 2018 Mar;15(3 Pt A):408-414.
- Brekelmans CTM, Saynaeve C, Bartels CC, et al. Effectiveness of breast cancer surveillance in BRCA1/2 gene mutation carriers and women with high familial risk. J Clin Oncology. 2001;19;924-930.
- Warner E. Screening BRCA1 and BRCA2 mutation carriers for breast cancer. Cancers (Basel). 2018;10(12):477.
- Lee JM, McMahon PM, Kong CY, et al. Cost-effectiveness of breast MR imaging and screen-film mammography for screening BRCA1 gene mutation carriers. Radiology. 2010;254(3):793-800.
- Warner E Messersmith H, Causer P, et al. Systematic review: Using MRI to screen women at high risk of breast cancer. Ann Int Medicine. 2008;148:671-679.
- Daly MB. PIlarski R, Berry MP, Buys SS et al. Genetic/familial high risk assessment: breast and ovarian cancers. Version 2.2019. Available at
https:///www.nccn.org/professionals/physician .
- Rowley H. To be alarmed or not to be alarmed over gadolinium contrast revelations: That is the question. European Congress in Radiology 2017 Annual Meeting. Available at
- BIRI Registry for Development and Validation of Novel MR Imaging Techniques, Cedars-Sinai Medical Center PI Dr Debaio Li (correspondence)
- Shahrouki P, Moriarty JM, Khan SN, et al. High resolution, 3-dimensional Ferumoxytol-enhanced cardiovascular magnetic resonance venography in central venous occlusion. J Cardiovasc Magn Reson. 2019 Mar 11;21(1):17.
- Bird S, Gelperin K, Sahin L et al. First-trimester exposure to gadolinium-based contrast agents: a utilization study of 4.6 million U.S. pregnancies. Radiology. 2019 Aug 20:190563.
doi: 10.1148/radiol.2019190563 . [Epub ahead of print]
Articles in this issue
over 6 years ago
Readers React: SCD and the work of Dr. Doris Wethersover 6 years ago
Alternatives to traditional surgery for fibroidsover 6 years ago
Has gestational hypertension been banished?over 6 years ago
Substance use in the breastfeeding womanover 6 years ago
When seven surgeries equal one lawsuitover 6 years ago
Vaginal gel shows promise for recurrent BVover 6 years ago
Urologic chronic pelvic pain syndrome and female sexual functionover 6 years ago
Age at menopause and type 2 diabetesNewsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.