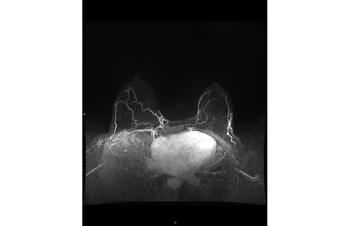
MRI scoring system for adnexal masses
Findings from JAMA Network Open indicate that a magnetic resonance imaging (MRI)-based system could be effective for assessing adnexal masses that are indeterminate on ultrasonography.
European investigators say that results of a new multicenter study suggest that a magnetic resonance imaging (MRI)-based system could be effective for assessing adnexal masses that are indeterminate on ultrasonography. The
O-RADS-MRI (ovarian-adnexal reporting data system magnetic resonance imaging) was previously tested in a retrospective single-center study. The new research was done prospectively in a much larger cohort and the findings, according to the authors, support publication of Version 1 of O-RADS-MRI.
Methods
To validate use of the technology, the researchers conducted a cohort study at 15 referral centers from March 1, 2013 to March 31, 2016. The patients were undergoing expectant management of an adnexal mass and 2-year follow-up data on them were completed by March 31, 2018.
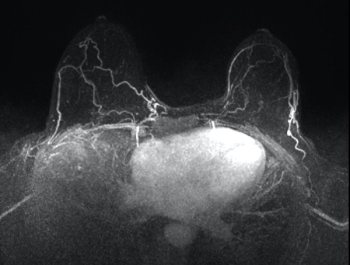
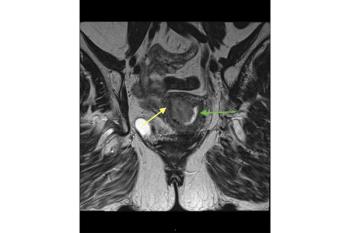
The cohort underwent routine pelvic MRI for characterization of a sonographically indeterminate adnexal mass, according to routine diagnostic practice at the centers. The O-RADS-MRI score was prospectively applied by two onsite readers and one reader and one reader masked to clinical and ultrasonography data. Scoring was on a 5-point scale, with categories reflecting the positive likelihood ratio for malignant neoplasm.
In the earlier retrospective study, a diagnostic score of 2 was associated with a less than 2% risk of malignancy, whereas a score of 4 or higher had sensitivity and specificity for malignancy of 93.5% and 96.6%, respectively. The system was designed to relay the radiologist’s suspicions to the clinician and help standardize reporting of MRI imaging findings.
Findings
A total of 1340 women aged 18 to 96 were enrolled in the current study. Of the 1194 who were evaluable, 1130 (94.6%) had a pelvic mass on MRI with a reference standard (surgery, 68 [67.9%]; 2-year follow-up, 362 [32.1%]). A total of 203 patients (18.0%) had at least one malignant adnexal or nonadnexal pelvic mass.
No invasive cancer was assigned a score of 2. Positive likelihood ratios were 0.01 for score 2, 0.27 for score 3, 4.42 for score 4, and 38.81 for score 5. Area under the receiver operating characteristic curve was 0.961 (95% CI, 0.948-0.971) among experienced readers, with a sensitivity of 0.93 (95% CI, 0.89-0.96; 189 or 203 patients) and a specificity of 0.91 (95% CI, 0.89-0.93; 848 of 927 patients).
There was good interrater agreement among both experienced and junior readers (Ï° = 0.784; 95% CI, 0.743 -0.824). Of 580 of 1130 women (51.3%) with a mass on MRI and no specific gynecological symptoms, 362 (62.4%) underwent surgery. Of them, 244 (67.4% had benign lesions and a score of 3 or less.
Conclusions
The MRI score correctly reclassified the mass origin as nonadnexal with a sensitivity of 0.99 (95% CI, 0.98-0.99; 1360 of 1372 patients) and a specificity of 0.78 (95% CI, 0.71-0.85); 102 of 130 patients). According to the authors, “The MRI score may provide potentially crucial information for determining the therapeutic strategy, allowing the risks and benefits of expectant management or surgery to be considered case by case.”
Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.