
In a recent study, the association between poor prenatal diet and adiposity outcomes in children was directly impacted by prenatal psychosocial stress.

In a recent study, the association between poor prenatal diet and adiposity outcomes in children was directly impacted by prenatal psychosocial stress.

“Vaccination coverage among pregnant women remains a priority,” the study authors noted.

The relationship between cesarean sections and childhood asthma has been investigated before, however, previous results have yielded conflicting evidence.

These findings may be useful for providers to practice shared decision-making with women regarding PPI use in early pregnancy.

Findings from a study in JAMA Network Open reveal valuable insight into the way cannabis legalization has impacted the perceptions of pregnant women who use cannabis in the US.

Alabama’s attorney general retracted comments he made last week suggesting criminal prosecution for women taking abortion pills for pregnancy termination. He is now saying that only providers who prescribe the pills could be prosecuted.

The Food and Drug Administration (FDA) has approved another Tdap vaccine option for use during pregnancy to prevent pertussis, otherwise known as whooping cough.
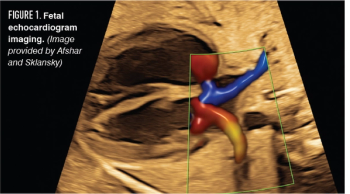
A review of the risks, benefits, and indications for appropriate referral of fetal echocardiography

While access to prenatal care did increase in states after Medicaid expansion, disparities persisted and even increased among Asian and Hispanic immigrant pregnant women, according to an analysis in JAMA Network Open.

After the Antenatal Late Preterm Steroid (ALPS) trial showed a decrease in respiratory complications following steroid administration, steroid exposure among newborns increased.

Testing the ratio between 2 placental proteins may be an early predictor of women at risk of developing preeclampsia with severe features.
Jeanette Carpenter, MD, MSCI, maternal-fetal medicine specialist at Pediatrix Medical Group, discussed a recently published study regarding pregnant COVID-19 patients who also had disseminated intravascular coagulation (DIC).
Bacterial vaginosis during pregnancy may lead to increased risks for preterm birth, preterm delivery, and spontaneous abortion, according to new research in the Archives of Gynecology and Obstetrics.

A recent study found that children born to mothers who had consumed caffeine during pregnancy often had a reduced height during childhood compared with those born to mothers who had not consumed caffeine.

Women in the US are more likely to be murdered during pregnancy or soon after childbirth than to die from the country’s top 3 leading causes of maternal death—high blood pressure disorders, hemorrhage, or sepsis—according to research in The BMJ.

Why obstetrics and gynecology is seeing an increase in applicants

Mothers with gestational diabetes experienced a lower rate of adverse perinatal outcomes if they achieved glycemic control within the first 8 weeks of diagnosis, according to the results of a new study.

Among pregnant women coinfected with HIV, a higher hepatitis C viral load increased the likelihood of transmitting HCV to children.

Although the proportion of women treated with biologics continues to grow, data on treatment recommendations among both physicians and female patients of childbearing age remain limited.
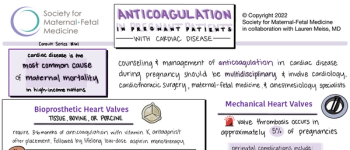
View the latest recommendations from the Society for Maternal-Fetal Medicine on anticoagulation in pregnant patients with cardiac disease.

Investigators found that women in states with child abuse or mandated reporting policies were less likely to visit prenatal care and postpartum health care.

As the COVID-19 pandemic continues, now in its third year, we have learned and continue to learn much about the cardiovascular complications that arise as a result of the novel coronavirus infection.

In a recent study, offspring delivered through cesarean section were more likely to develop Crohn’s disease than those vaginally delivered.

Prenatal exposure to industrial air pollutants increases risk of adverse birth outcomes in infants.

In a recent study, prenatal cannabis exposure was associated with greater risk of behavioral problems and mental health disorders in children.