
Menopausal Hormone Therapy and Other Breast Cancer Risk Factors in Relation to the Risk of Different Histological Subtypes of Breast Cancer: A Case-control Study

Menopausal Hormone Therapy and Other Breast Cancer Risk Factors in Relation to the Risk of Different Histological Subtypes of Breast Cancer: A Case-control Study

In humans, serotonin has typically been investigated as a neurotransmitter. However, serotonin also functions as a hormone across animal phyla, including those lacking an organized central nervous system.

Breast cancer is a growing concern among premenopausal women. With an emphasis on this patient population, this article discusses the known risk factors for breast cancer; models for quantitative risk assessment; and strategies for modifying breast cancer risk, including screening mammography, prophylactic mastectomy, and primary pharmacologic prevention.

Postmenopausal osteoporosis is a major health problem, primarily because of the severe morbidity and mortality associated with osteoporotic fractures.

The age at which a woman reaches menopause is 85% genetically determined, according to new research published Thursday, in Europe's leading reproductive medicine journal, Human Reproduction*.

A report just published in the Journal of the American Medical Association confirmed previous studies which found that women who take hormone replacement therapy (HRT) may develop denser breast tissue, which in turn may make it more difficult to detect breast cancer through mammography.

Both the estrogen receptor (ER) and vitamin D receptor (VDR) belong to the same superfamily of nuclear receptors and both receptors are activated by interaction with their ligands.

Healthy, nonsmoking perimenopausal women can derive a host of benefits from using oral contraceptives (OCs). Along with providing effective contraception, OCs can regulate their menstrual cycles, reduce hot flashes, and protect against two gynecologic cancers.

Like the proverbial elephant, osteoporosis has been described in ways that vary according to the scientific orientation of the describer. It has been defined clinically as the presence of fracture; biomechanically as decreased bone strength; radiographically as osteopenia; histomorphometrically as reduced bone matrix per unit of bone volume; and epidemiologically as increased fracture risk.

There are many ways to take estrogens and many philosophies of management. The views expressed on this page represent the opinion of the author and may or may not conform to the current "standard of care" prevalent in the United States today.

A 27-year study of 1300 women undergoing retropubic cystourethropexy using either the modified Marshall-Marchetti-Krantz procedure or the modified Pereyra procedure compares long-term results when the type of surgery is selected on the basis of patient criteria.

In many mammals, the duration of the nocturnal melatonin elevation regulates seasonal changes in reproductive hormones such as luteinizing hormone (LH). Melatonin's effects on human reproductive endocrinology are uncertain.

Natural Estrogens, Selective Estrogens, Fantasy Estrogens... What is the Perfect Estrogen?

Perhaps the principal reason male menopause has never been in the public spotlight is because men who experience the characteristic decline in virility during middle age are reluctant or even unwilling to acknowledge the condition.

This is adapted from an interview with Dr. Howard Glazer, who has developed a treatment for this condition using a form of biofeedback. This initial interview, covers the history of the disease, as well as Dr. Glazer's background.

The Treatment of Vulvovaginal Pain Disorders with Surface Electromyographic Assisted Pelvic Floor Muscle Rehabilitation

Receiving a diagnosis of cancer is a major life change. Neither the patient, the family nor friends will be the same again.

Body Mass Index, Percent Body Fat, and Regional Body Fat Distribution in Relation to Leptin Concentrations in Healthy, Non-Smoking Postmenopausal Women in a Feeding Study

The post marketing safety surveillance program for a drug containing a new chemical entity should assess both, the safety outcomes that relate specifically to the targeted population, as well as those that could potentially be related to special pharmacological characteristics of the drug.

Human, animal, and in vitro research indicates a beneficial effect of appropriate amounts of omega-3 (n-3) polyunsaturated fatty acids (PUFA) on bone health.

Many risk factors for fractures have been documented, including low bone-mineral density (BMD) and a history of fractures.

Urinary incontinence impacts 15 to 35% of the adult ambulatory population. Men after the removal of the prostate for cancer can experience incontinence for several weeks to years after the surgery.

Diagnostic discordance for osteoporosis is the observation that the T-score of an individual patient varies from one key measurement site to another, falling into two different diagnostic categories identified by the World Health Organization (WHO) classification system.
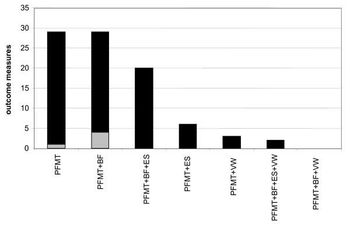
Stress urinary incontinence (SUI) is a prevalent and costly condition which may be treated surgically or by physical therapy.

The relationship of sex hormones and breast cancer is a matter of concern of many women. Breast cancer is the most common form of cancer in women in industrialized countries.